Urinary problems pop up for lots of reasons — infections, prostate issues, stones, overactive bladder, or even diabetes. This short guide tells you the common signs, easy things to try at home, and the red flags that mean you should see a clinician right away.
If you get burning when peeing, more trips to the bathroom, cloudy or strong-smelling urine, think UTI. A weak stream, hesitancy, or dribbling often points to prostate enlargement in men. Sudden, severe side or back pain with blood in the urine may mean a kidney stone. If you leak when you sneeze, cough, or laugh, that’s stress incontinence; sudden, strong urges to go and leaking after rushing to the toilet is overactive bladder. Long-term conditions like diabetes, neurological problems, or some medicines can also affect bladder control.
Some symptoms need fast care: fever over 38°C (100.4°F), severe pain, vomiting, confusion, fainting, or heavy bleeding in urine. These can signal a serious infection or complication — go to urgent care or the ER.
Drink steady amounts of water through the day. Proper hydration helps flush bacteria and reduces irritation. Cut back on caffeine, alcohol, and fizzy drinks for a few days to see if symptoms ease — they can make urgency and leakage worse.
Use good bathroom habits: empty the bladder fully, sit to pee if that helps, and try timed voiding (every 2–4 hours) to retrain an overactive bladder. For women, wipe front to back and urinate after sex. Avoid harsh soaps or douches near the genitals; choose cotton underwear and loose clothing.
Pelvic floor exercises help both women and men with leakage. Squeeze the muscles you use to stop urine for 3–5 seconds, repeat 10 times, three times a day. Many people notice improvement in a few weeks.
Over-the-counter phenazopyridine can reduce burning for a day or two but won’t treat an infection. Cranberry products may help prevent some UTIs for some people, but they’re not a cure. If you suspect a UTI, see a clinician for urine testing and appropriate antibiotics.
If problems repeat, keep a short bladder diary: note fluid intake, bathroom times, leakage, and triggers like coughing or sneezing. That info helps your doctor pick the right tests and treatments faster. Your provider may order urine tests, blood sugar checks, imaging, or refer you to a urologist or pelvic floor therapist.
When buying meds or seeking advice online, use sites and pharmacies that require prescriptions and show clear contact info. TotalCareMart Pharmaceutical Guide aims to point you toward safe info, but personal care decisions need a real provider.
Small habits matter: regular hydration, timed voiding, pelvic exercises, and avoiding bladder irritants can cut symptoms for many people. Track changes, get checked when things feel off, and ask for help before a simple issue becomes a serious one.
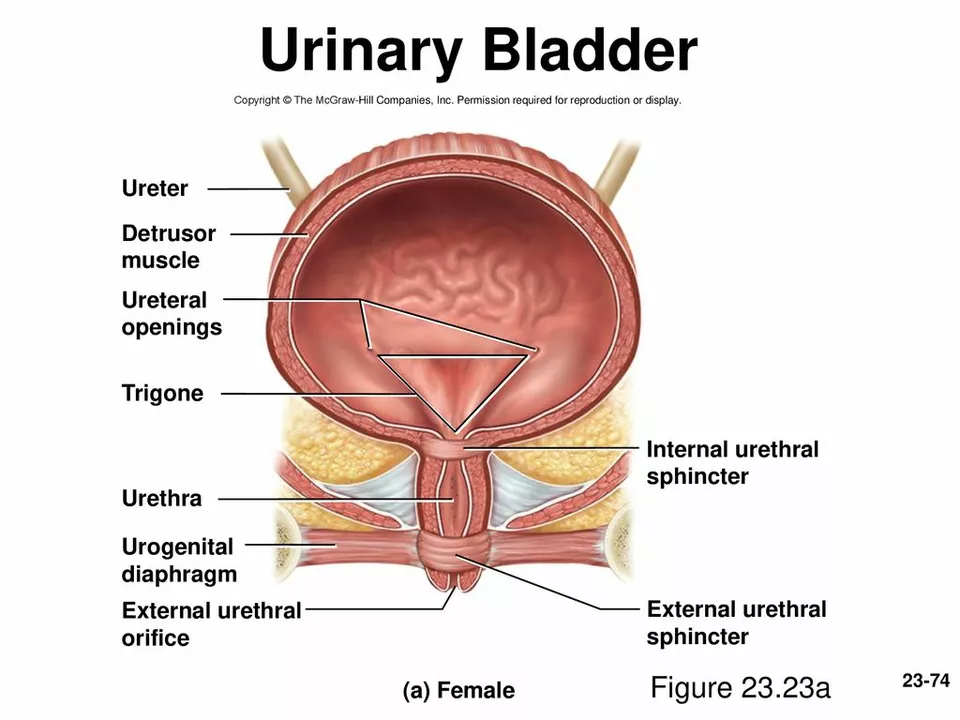
As someone who has been researching bladder health, I recently discovered the connection between bladder prolapse and difficulty urinating. Bladder prolapse, also known as cystocele, occurs when the bladder's supportive tissue weakens, causing it to drop and press against the vaginal wall. This can lead to difficulty urinating, as the bladder's position and function may be compromised. In some cases, this may result in incomplete emptying of the bladder and an increased risk of urinary tract infections. It's important to be aware of this connection and seek medical advice if you're experiencing any difficulty urinating or other related symptoms.