Understanding Bladder Prolapse and Its Symptoms
Bladder prolapse, also known as cystocele, is a common condition among women, especially those who have given birth or experienced menopause. It occurs when the bladder drops from its normal position and pushes against the vaginal wall. This can cause a wide range of symptoms, one of which is difficulty urinating. In this article, we will explore the connection between bladder prolapse and difficulty urinating, as well as other symptoms and complications that may arise.
How Bladder Prolapse Leads to Difficulty Urinating
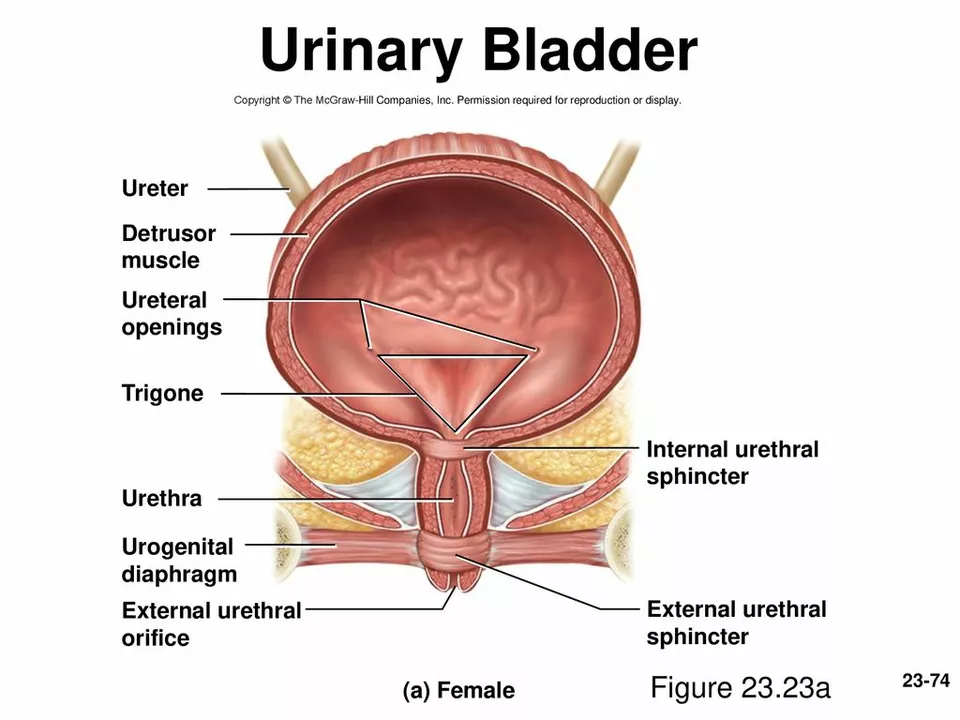
When the bladder prolapses, it can cause a kink or obstruction in the urethra, making it difficult for urine to flow freely. This can result in several urinary issues, such as incomplete emptying of the bladder, frequent or urgent need to urinate, and even urinary incontinence. This difficulty in urination can be both frustrating and uncomfortable, impacting a person's overall quality of life.
Other Symptoms of Bladder Prolapse
Besides difficulty urinating, bladder prolapse can also cause other symptoms. Some of these include a feeling of pressure or discomfort in the pelvic region, a bulge in the vagina, lower back pain, and painful intercourse. These symptoms can vary in severity depending on the degree of prolapse and may worsen during certain activities such as lifting heavy objects or standing for long periods.
Factors That Increase the Risk of Bladder Prolapse
There are several factors that can increase the risk of developing bladder prolapse. These include age, childbirth, obesity, chronic constipation, and heavy lifting. Women who have gone through menopause or have had a hysterectomy are also at a higher risk due to the decrease in estrogen levels, which can weaken the pelvic floor muscles and supportive tissues.
Diagnosing Bladder Prolapse
If you suspect that you may have bladder prolapse, it is important to consult with a healthcare professional for proper diagnosis and treatment. A physical examination, including a pelvic exam, will typically be performed to evaluate the degree of prolapse and check for any other pelvic disorders. Additional tests, such as a bladder function test or imaging studies, may also be ordered to assess the severity of the condition and rule out other issues.
Treatment Options for Bladder Prolapse
Fortunately, there are several treatment options available for bladder prolapse, depending on the severity of the condition and the patient's preferences. For mild cases, conservative treatments such as pelvic floor exercises (Kegel exercises), weight loss, and avoiding heavy lifting may be recommended. In more severe cases, a pessary (a device inserted into the vagina to support the bladder) or surgical intervention may be necessary to correct the prolapse and alleviate symptoms.
The Role of Pelvic Floor Exercises
Pelvic floor exercises, or Kegel exercises, can help strengthen the muscles that support the bladder and other pelvic organs. By practicing these exercises regularly, you may be able to improve bladder control and reduce the symptoms of bladder prolapse. It is important to consult with a healthcare professional to learn the proper technique for performing Kegel exercises and to ensure that they are appropriate for your specific situation.
Preventing Bladder Prolapse and Difficulty Urinating
While not all cases of bladder prolapse can be prevented, there are certain measures that can be taken to reduce the risk or slow the progression of the condition. These include maintaining a healthy weight, practicing pelvic floor exercises, avoiding heavy lifting, and treating chronic constipation. Additionally, seeking prompt medical care for any urinary or pelvic symptoms can help ensure that any underlying issues are addressed before they worsen.
Living with Bladder Prolapse and Difficulty Urinating
Bladder prolapse and the associated difficulty urinating can significantly impact a person's quality of life. However, with proper diagnosis, treatment, and self-care measures, many individuals are able to manage their symptoms and lead active, fulfilling lives. It is essential to work closely with your healthcare provider to develop a personalized treatment plan and to ask any questions you may have about living with bladder prolapse.

Ben Poulson
May 27 2023Pelvic floor integrity plays a pivotal role in urinary function, and a cystocele frequently disrupts this balance. When the bladder descends, the urethral angle can be altered, leading to incomplete emptying or a sense of urgency. Strengthening the levator ani muscles through structured Kegel regimens often mitigates these symptoms. Additionally, weight management reduces intra‑abdominal pressure that exacerbates prolapse. Clinical assessment should include a standardized POP‑Q grading to guide therapeutic decisions. Non‑surgical options remain first‑line for mild presentations, while severe cases may warrant pessary fitting or surgical suspension. Early intervention is essential to preserve quality of life.