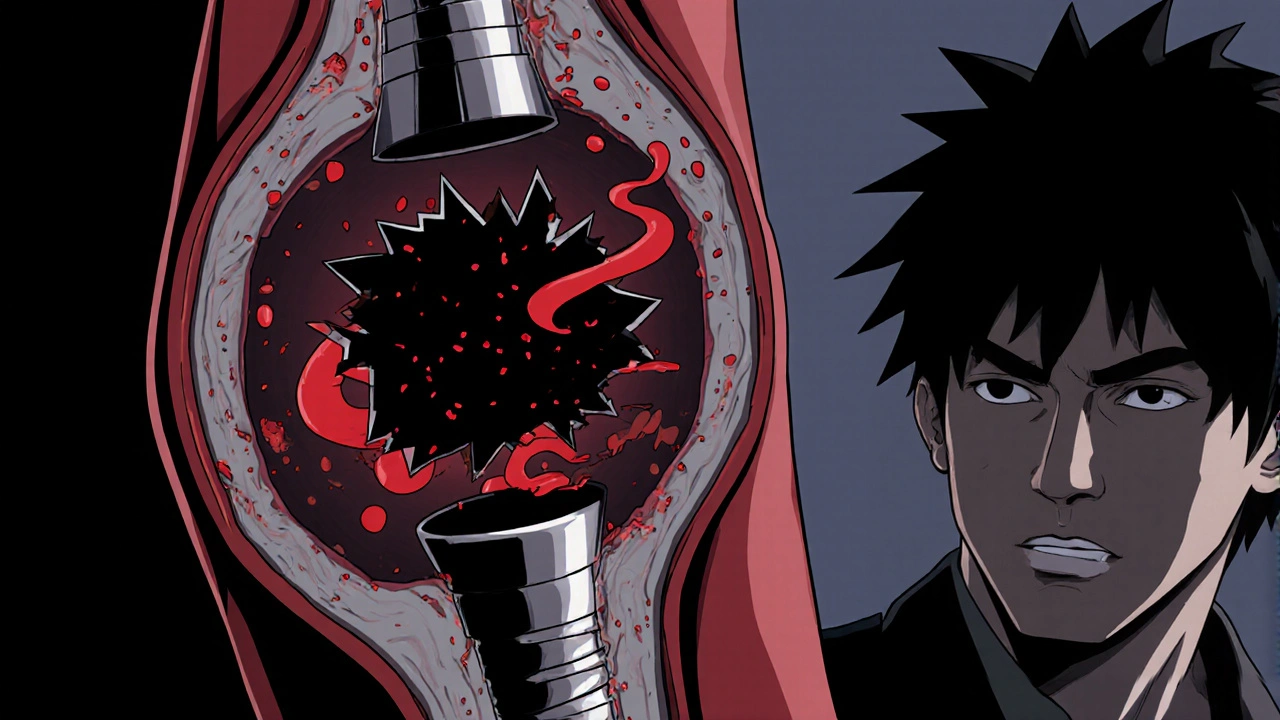
When you hear the term stent thrombosis, the formation of a blood clot inside a coronary stent that can block blood flow and trigger a heart attack. Also known as in‑stent thrombosis, it is a serious complication that can happen after a heart procedure. Most often it follows a percutaneous coronary intervention, a minimally invasive technique where a balloon and a stent are used to reopen a narrowed artery. The stent acts like a tiny scaffold, keeping the artery open, but if a clot forms on its surface the benefits disappear in minutes. Understanding why this clot forms, who is most at risk, and how doctors try to stop it is the first step toward keeping your heart safe.
One major driver of stent thrombosis is the underlying coronary artery disease, the buildup of fatty plaque that narrows the heart's blood vessels. Plaque can rupture, exposing a sticky surface that encourages clotting. When a stent is placed, the artery wall is injured, and the body’s natural healing response can overshoot, leading to a clot. To counter this, doctors prescribe dual antiplatelet therapy, a combination of aspirin and a second antiplatelet drug that keeps platelets from sticking together. This regimen is usually required for at least six months after the procedure, and the exact length depends on the type of stent and the patient’s risk profile. The kind of stent matters too. drug‑eluting stents, stents that slowly release medication to prevent the artery from re‑narrowing (restenosis) have lowered the need for repeat procedures, but some studies show they may alter the clotting environment, making careful medication management even more important. In contrast, bare‑metal stents tend to heal faster but carry a higher risk of restenosis, which can also set the stage for a clot. Other risk factors include diabetes, smoking, high cholesterol, and a history of clotting disorders. Lifestyle tweaks—quitting tobacco, eating a heart‑healthy diet, staying active—and controlling blood sugar and lipids all play a role in reducing the chance of a clot forming inside the stent. Below you’ll find a curated list of articles that dive deeper into each of these topics. From the science behind coronary artery disease to practical tips on adhering to dual antiplatelet therapy, and comparisons of stent types, the posts aim to give you clear, actionable information. Whether you’re a patient trying to understand your treatment plan or a caregiver looking for ways to support someone after a PCI, the collection offers insights that can help you manage and prevent stent thrombosis. Explore the guides below to see how each piece fits into the bigger picture of heart health.
Practical stress‑management techniques that lower the chance of blood clots forming in heart stents and boost overall heart health.