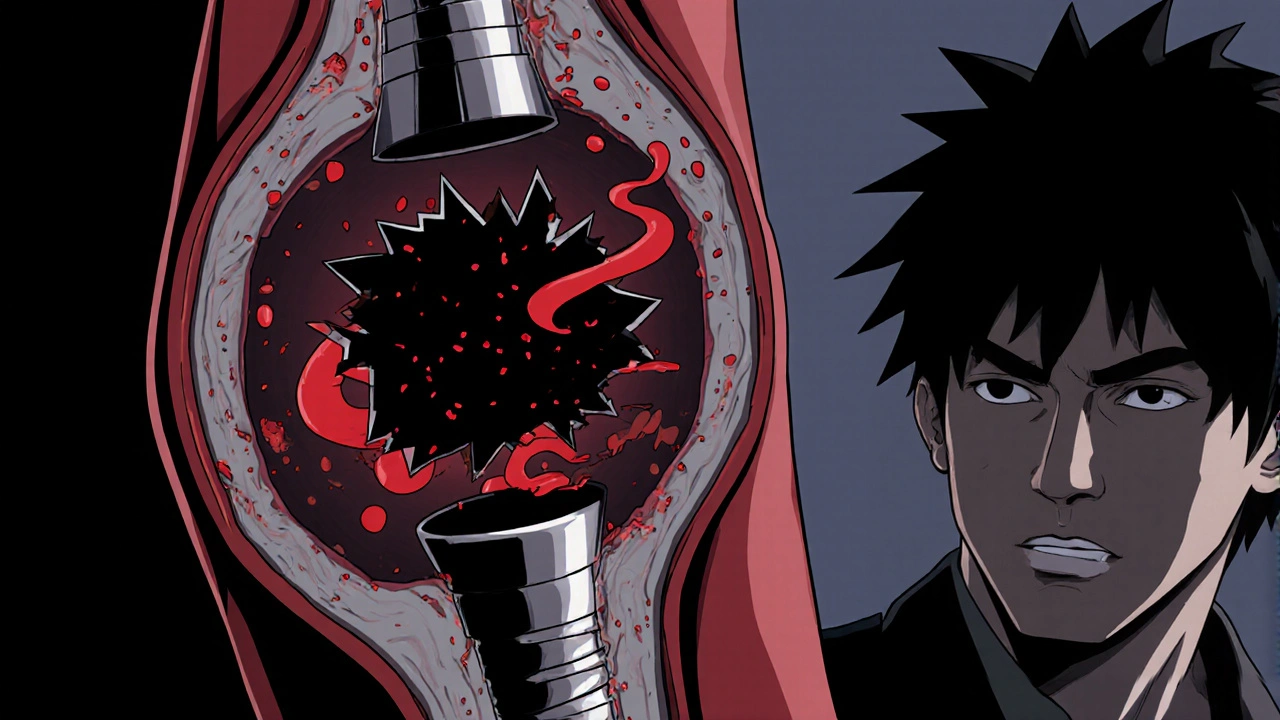
When a coronary stent thrombosis occurs, a blood clot forms inside the metal mesh that keeps a previously narrowed artery open. It’s a serious complication that can trigger a heart attack or even be fatal. While doctors prescribe antiplatelet drugs and recommend healthy habits, one often‑overlooked factor is stress. Chronic stress spikes hormones like cortisol, fuels inflammation, and makes platelets more “sticky.” Managing that stress can meaningfully stress management reduce the odds of a clot forming in your stent.
What Is Stent Thrombosis and Why Does It Matter?
A stent is a tiny metal or polymer tube implanted during angioplasty to prop open a clogged coronary artery. Stent thrombosis describes a clot that develops inside the stent, obstructing blood flow. The risk is highest in the first month after implantation but never disappears entirely. Key medical risk factors include:
- Premature discontinuation of antiplatelet therapy
- Diabetes, hypertension, and high cholesterol
- Smoking and excessive alcohol
- Elevated inflammatory markers (e.g., CRP)
- Persistent psychological stress
How Stress Fuels Clot Formation
The body’s stress response is designed for short bursts: adrenaline surges, heart rate climbs, and blood vessels constrict to prepare for “fight or flight.” When stress becomes chronic, the system stays turned on, leading to three main pathways that promote clotting:
- Cortisol overload: Prolonged cortisol release raises blood glucose and triglyceride levels, making the blood thicker.
- Inflammation escalation: Stress triggers cytokines such as IL‑6 and TNF‑α, which activate the endothelial lining of arteries and attract platelets.
- Platelet hyper‑reactivity: Studies show that people under chronic stress have 15‑30% higher platelet aggregation, meaning clots form faster.
These mechanisms intersect: higher cortisol fuels inflammation, which in turn sensitizes platelets. The result is a perfect storm inside a stent, where the metal surface already encourages platelet adhesion.
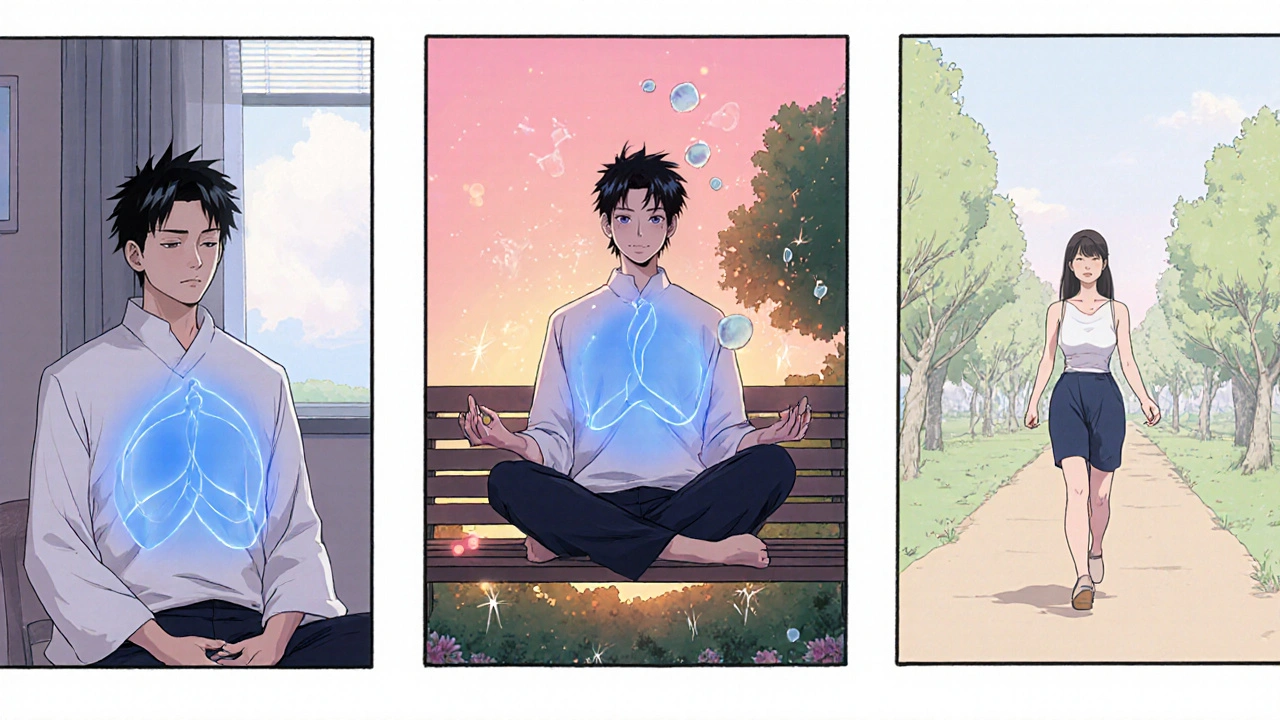
Core Stress‑Management Techniques That Impact Clot Risk
Not every stress‑relief method works the same for heart health. Here are the ones backed by clinical or physiological data:
- Mindful breathing: Slow, diaphragmatic breaths (4‑7‑8 technique) lower heart rate variability and reduce cortisol within 10 minutes.
- Daily meditation: A meta‑analysis of 20 trials found a 12% drop in systolic blood pressure and a modest reduction in CRP after 8 weeks of 20‑minute sessions.
- Regular aerobic exercise: 30 minutes of brisk walking improves endothelial function and cuts platelet aggregation by up to 22%.
- Sleep hygiene: Getting 7‑8 hours of uninterrupted sleep restores the nightly cortisol dip, lowering overall inflammation.
- Social connection: Positive relationships buffer stress hormones; a 2023 Australian cohort study linked weekly family meals to a 10% lower stent‑thrombosis rate.
Combining these practices creates a layered defense against the clot‑forming cascade.
Integrating Stress Management With Traditional Heart‑Care
Any stress‑reduction plan should sit alongside your doctor‑prescribed regimen. Typical medical pillars include:
- Antiplatelet therapy (e.g., aspirin + clopidogrel) - keep it consistent unless a clinician advises otherwise.
- Blood‑pressure control - ACE inhibitors or beta‑blockers.
- Cholesterol management - statins.
When you add stress‑management tactics, the combined effect is synergistic. For example, exercising not only lowers blood pressure but also releases endorphins that curb anxiety, making you more likely to stick with medication schedules.
Step‑by‑Step Daily Routine to Lower Clot Risk
- Morning check‑in (5 min): Sit upright, close eyes, and do the 4‑7‑8 breathing cycle three times.
- Medication audit (2 min): Verify you’ve taken your antiplatelet pills with water.
- 30‑minute walk or bike ride (30 min): Aim for moderate intensity-talking should be possible but slightly challenging.
- Mid‑day mindfulness break (10 min): Use a guided meditation app or simply focus on ambient sounds.
- Balanced lunch: Include omega‑3 rich foods (salmon, walnuts) that combat inflammation.
- Afternoon stretch (5 min): Neck rolls, shoulder shrugs, and light calf raises to keep circulation flowing.
- Evening wind‑down (30 min before bed): Dim lights, avoid screens, and journal any stressful thoughts to externalize them.
- Sleep routine (7‑8 h): Keep a consistent bedtime, use a cool dark room, and consider a white‑noise machine.
Mark each activity on a simple daily tracker; consistency is the key metric that predicts reduced clot risk.
Quick Checklist - Reduce Clot Risk in Stents
- Never skip antiplatelet medication.
- Practice 4‑7‑8 breathing twice daily.
- Walk or jog at least 150 minutes a week.
- Meditate for 20 minutes, 4 times a week.
- Prioritize 7‑8 hours of sleep.
- Eat omega‑3 rich foods and limit processed sugars.
- Stay hydrated - 2‑3 liters of water daily.
- Reach out to friends or support groups weekly.

When to Seek Professional Help
If you notice any of the following, contact your cardiologist promptly:
- Chest discomfort or pressure that lasts more than a few minutes.
- Sudden shortness of breath at rest.
- Unexplained dizziness or palpitations.
- Persistent high stress that feels unmanageable despite self‑help strategies.
Early medical intervention can prevent a clot from becoming a full‑blown heart attack.
Table: Stress‑Reduction Techniques & Their Measured Impact on Clot‑Related Markers
| Technique | Typical Session Length | Observed Change in Cortisol | Effect on Platelet Aggregation | Impact on CRP (Inflammation) |
|---|---|---|---|---|
| 4‑7‑8 Breathing | 5 min | ‑12% after one session | ‑5% (short‑term) | Neutral |
| Guided Meditation | 20 min, 4×/wk | ‑18% after 8 weeks | ‑15% | ‑10% |
| Aerobic Exercise | 30 min, 5×/wk | ‑8% (baseline) | ‑22% | ‑7% |
| Sleep Optimization | 7‑8 h/night | ‑15% (restful nights) | ‑10% | ‑12% |
| Social Engagement | Weekly | ‑10% (average) | ‑8% | ‑9% |
Frequently Asked Questions
Can stress alone cause a clot in my stent?
Stress isn’t the only cause, but chronic stress amplifies the same biological pathways-cortisol, inflammation, platelet activation-that lead to clot formation. Combined with other risk factors, it can tip the balance toward thrombosis.
How soon will I see benefits from stress‑management practices?
Some benefits, like a lower heart rate and reduced cortisol, appear after a single session of breathing or meditation. More lasting changes-reduced CRP, lower platelet reactivity-typically emerge after 4‑8 weeks of consistent practice.
Do I need a therapist, or can I self‑manage stress?
Mild to moderate stress can often be handled with self‑guided techniques-breathing, apps, exercise. If you notice persistent anxiety, sleep disruption, or mood swings, a mental‑health professional can tailor a program and monitor progress.
Will stress‑reduction interfere with my heart medication?
No. In fact, lower stress can improve medication adherence and may enhance drug effectiveness by reducing inflammatory interference. Always keep your cardiologist in the loop about any new routine.
Is there a specific diet that works best with stress management?
A Mediterranean‑style diet-rich in oily fish, nuts, olive oil, fresh veggies, and whole grains-provides omega‑3 fatty acids and antioxidants that blunt inflammation and support brain chemistry, making stress easier to handle.

Samantha Vondrum
October 23 2025Effective stress mitigation can directly influence platelet activity, thereby reducing stent thrombosis risk 😊. By incorporating diaphragmatic breathing and brief mindfulness sessions into daily routines, patients create a measurable decline in cortisol levels, which in turn dampens inflammatory cascades. It is essential to coordinate these practices with prescribed antiplatelet therapy to achieve synergistic protection. Please consider sharing these strategies with your support network, as collective adherence amplifies outcomes.