When dealing with serotonin syndrome, a potentially life‑threatening condition caused by excessive serotonin activity in the brain and body. Also known as serotonergic toxicity, it often shows up after mixing certain medications or taking an overdose. A core component is serotonin, the neurotransmitter that regulates mood, temperature, and pain perception. The most common culprits are antidepressants, drugs that raise serotonin levels, including SSRIs, SNRIs, and MAOIs. Specific classes such as MAOIs, monoamine oxidase inhibitors that block serotonin breakdown and SNRIs, serotonin‑norepinephrine reuptake inhibitors that increase serotonin and norepinephrine are frequently cited in case reports. Understanding these relationships helps you spot the problem before it escalates.
Serotonin syndrome usually presents with a mix of mental, autonomic, and neuromuscular symptoms. Mentally, people may feel agitated, confused, or experience hallucinations. Autonomic signs include rapid heart rate, high blood pressure, sweating, and fever that can climb above 104°F. Neurologically, you might notice tremor, hyperreflexia, clonus, or even muscle rigidity. The classic “triad” – altered mental status, autonomic instability, and neuromuscular hyperactivity – is a reliable clue for clinicians. Because the symptoms can mimic infections or drug overdose, a careful medication history is essential to make the correct diagnosis.
Diagnosis relies on clinical criteria rather than lab tests. The Hunter Serotonin Toxicity Criteria are widely used: if a patient has taken a serotonergic agent and shows spontaneous clonus, inducible clonus plus agitation, ocular clonus, or hyperreflexia with temperature above 38°C, the diagnosis is likely. Blood tests may show elevated creatine kinase from muscle breakdown, but they’re not definitive. Imaging is rarely needed unless complications like rhabdomyolysis arise. The key is linking the symptom pattern to recent drug exposure, which underscores the importance of a thorough medication review.
Treatment is a race against time. The first step is to stop all serotonergic drugs immediately. Supportive care follows: cooling measures for hyperthermia, IV fluids to maintain blood pressure, and benzodiazepines to calm agitation and reduce muscle rigidity. In severe cases, serotonin antagonists like cyproheptadine are administered orally or via feeding tube. Intensive care may be required for patients with respiratory failure or organ damage. Early intervention dramatically lowers the risk of long‑term complications.
Prevention hinges on safe prescribing and patient education. Physicians should avoid combining multiple serotonergic agents whenever possible, especially mixing SSRIs with MAOIs or using high‑dose tramadol alongside antidepressants. When a switch between these drugs is necessary, a washout period—typically 14 days for MAOIs—helps the body clear excess serotonin. Patients should be told to report any new symptoms such as intense shivering, sudden confusion, or unusual muscle twitching right away. Pharmacists play a vital role by double‑checking prescriptions for risky combos.
Monitoring doesn’t stop at the pharmacy counter. If you’re starting a new antidepressant, schedule a follow‑up within a week to review side effects. Keep a written list of all medications, over‑the‑counter products, and supplements, because even herbal remedies like St. John’s wort can raise serotonin levels. For those with a history of serotonin syndrome, choosing non‑serotonergic treatments for pain or migraine may be safer. Knowing the warning signs and acting quickly can save lives.
Below you’ll find a curated set of articles that dive deeper into specific aspects of serotonin syndrome, from detailed case studies to practical guides on managing drug interactions. Use these resources to sharpen your understanding, recognize early signs, and apply safe treatment strategies in real‑world situations.
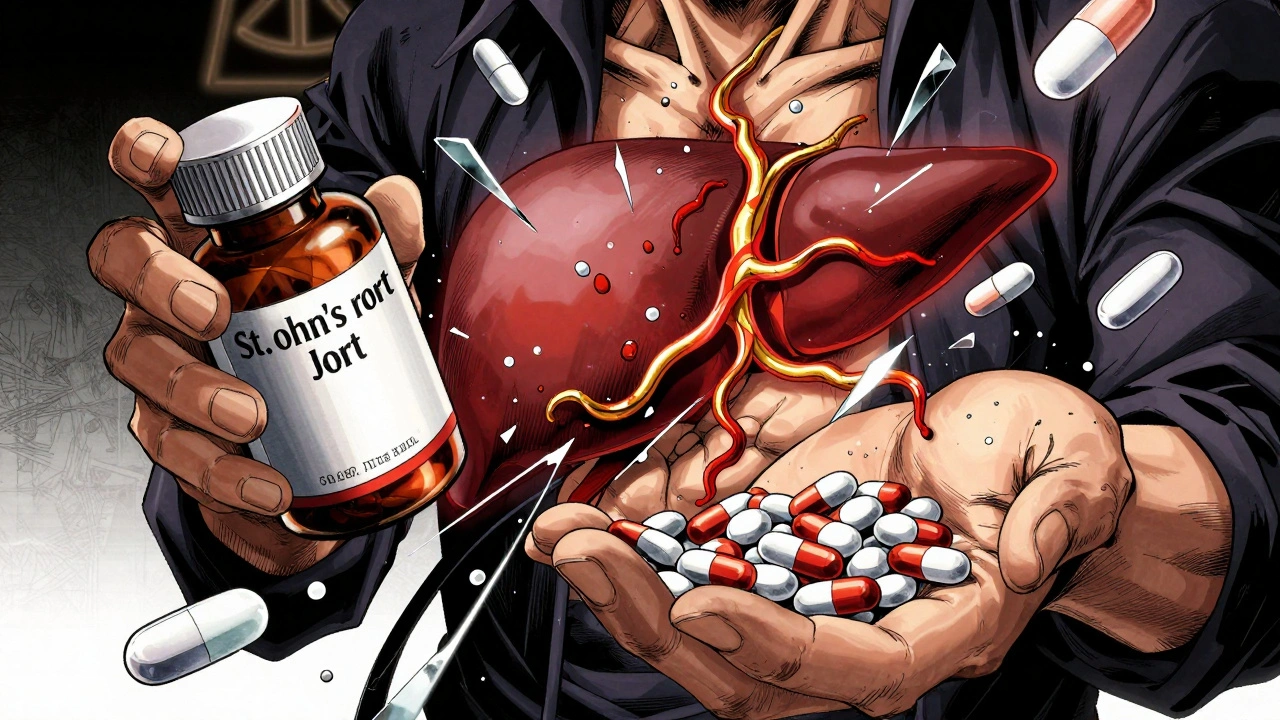
St. John's Wort may help mild depression, but it can make prescription drugs like warfarin, birth control, and antidepressants ineffective - or cause dangerous side effects. Learn which medications are at risk and what to do instead.

Learn how psychiatric medication interactions cause dangerous combos like serotonin syndrome and lithium toxicity, and get practical monitoring tips, checklists, and emerging tools to stay safe.