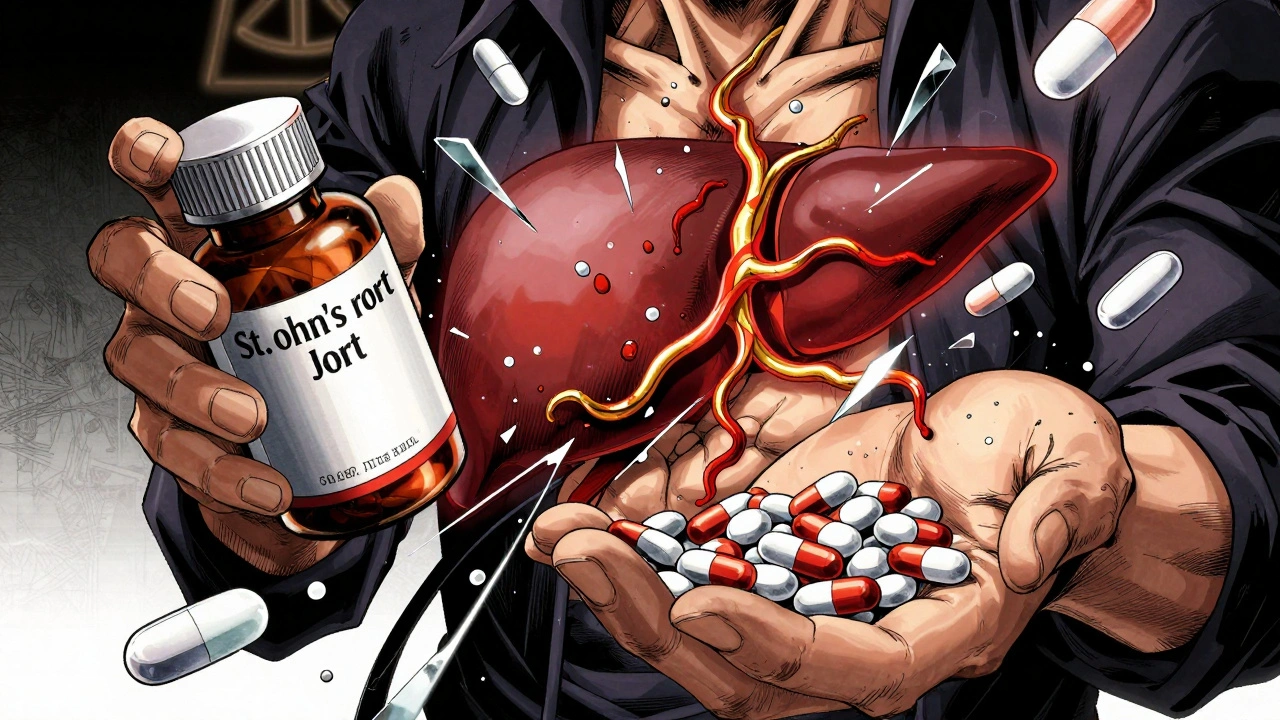
Many people turn to St. John’s Wort because it’s natural, affordable, and marketed as a gentle fix for low mood. But here’s the truth: St. John’s Wort isn’t harmless. It doesn’t just float through your body quietly. It actively changes how your prescription drugs work - sometimes dangerously so.
How St. John’s Wort Changes Your Medications
St. John’s Wort doesn’t just add to your meds. It rewires how your body processes them. Its main active ingredient, hyperforin, tricks your liver into cranking up production of enzymes like CYP3A4 and CYP2C9. These enzymes are your body’s cleanup crew for drugs. When they’re overworked, your medications get broken down too fast.
That means if you’re taking warfarin, cyclosporine, or birth control pills, your body may flush them out before they can do their job. Studies show blood levels of these drugs can drop by 30% to 50%. One patient on warfarin saw their INR - a key measure of blood thinning - plunge from 2.5 to 1.3 in just seven days after starting St. John’s Wort. That’s not a minor glitch. That’s a risk of stroke.
Drugs That Can Become Ineffective (or Dangerous)
St. John’s Wort doesn’t pick and choose. It hits a wide range of critical medications. Here’s what’s at risk:
- Anticoagulants like warfarin and phenprocoumon: Risk of blood clots, stroke, or heart attack.
- Immunosuppressants like cyclosporine and tacrolimus: Transplant rejection can happen fast - one patient lost their kidney graft after levels dropped 40%.
- HIV meds like saquinavir and efavirenz: Viral load can spike, leading to drug resistance and disease progression.
- Antidepressants like SSRIs (sertraline, fluoxetine) and nefazodone: This combo can trigger serotonin syndrome - a life-threatening surge in brain serotonin causing high fever, seizures, and irregular heartbeat.
- Birth control pills: Ethinyl estradiol levels drop 25-35%. There are documented cases of unplanned pregnancies in women taking pills perfectly - but also using St. John’s Wort.
- Anticonvulsants like carbamazepine and phenytoin: Seizures can return or worsen.
- Benzodiazepines like alprazolam (Xanax): Anxiety treatment fails because the drug is cleared too quickly.
- Statins like simvastatin and atorvastatin: Cholesterol control collapses. Pravastatin and fluvastatin are safer, but only because they’re metabolized differently.
- Digoxin: Heart failure can worsen as levels fall 25%.
- Theophylline: Asthma control fails, leading to ER visits.
There are over 50 documented major interactions. Some are rare. Others? Common enough that hospitals report one case every few months.
Why People Don’t Realize the Risk
Most people think, “It’s herbal. It’s natural. It can’t hurt.” That’s the biggest trap.
A 2022 Johns Hopkins study found that 41% of patients taking prescription drugs didn’t tell their doctor they were using St. John’s Wort. Why? Because they didn’t consider it a “medication.”
And it’s not just patients. Even some pharmacists miss it. A 2023 survey of U.S. hospitals showed 68% had dealt with a St. John’s Wort interaction in the last five years. The average cost per incident? Over $18,000 - not just in money, but in ER visits, hospital stays, and lost trust.
One Reddit user shared: “I took St. John’s Wort for 3 weeks while on birth control. I had breakthrough bleeding. Then I got pregnant. My OB said it was textbook.”

What Happens When You Stop Taking It?
Many assume the problem ends when they quit St. John’s Wort. It doesn’t.
Enzyme induction doesn’t vanish overnight. It takes up to two weeks for your liver to reset. So if you stop the herb and then restart your antidepressant or blood thinner without adjusting the dose, you could overdose.
One patient stopped St. John’s Wort after six weeks and restarted sertraline at their old dose. Within 48 hours, they were in the ER with tremors, confusion, and a fever of 103°F. Serotonin syndrome. They survived. But they didn’t know the delay could kill.
What Should You Do?
If you’re taking any prescription medication - even if it’s just one - don’t start St. John’s Wort without talking to your doctor or pharmacist.
If you’re already using it:
- Stop immediately and call your provider.
- Don’t just quit cold if you’re on an antidepressant - work with your doctor to taper safely.
- Ask for blood tests if you’re on warfarin, cyclosporine, digoxin, or anticonvulsants. Levels need to be checked 3-5 days after stopping or starting St. John’s Wort.
- Use a checklist. The University of Adelaide has a 57-item interaction list. Print it. Bring it to your next appointment.
And if you’re a patient: When your doctor asks, “Are you taking any other medications?” - say this: “I take St. John’s Wort for my mood.” Don’t say, “I take a natural supplement.” That’s not enough.

Is There a Safe Version?
Some companies now sell extracts labeled as “low hyperforin.” A 2023 study in Clinical Pharmacology & Therapeutics showed these versions caused far less enzyme induction while still helping mild depression.
But here’s the catch: The FDA doesn’t regulate supplements for purity or consistency. You can’t know what’s really in the bottle. A product labeled “low hyperforin” might still have enough to trigger an interaction.
The European Food Safety Authority put it bluntly: “No safe threshold can be established for patients on prescription drugs.”
Regulation Is All Over the Map
In Australia, St. John’s Wort products must carry a warning about drug interactions. In Germany and Sweden, you need a prescription. In the U.S., it’s sold like a vitamin - no warning required beyond a tiny disclaimer: “Ask a doctor if you’re taking prescription drugs.”
That’s not enough. In 2023, the FDA updated its guidance to demand stronger labeling, specifically naming warfarin, cyclosporine, and SSRIs. But many bottles still don’t comply.
The American Psychiatric Association’s 2023 guidelines went further: They removed St. John’s Wort from “may be considered” and moved it to “not recommended” for anyone on prescription meds.
What’s the Bottom Line?
St. John’s Wort might help mild depression. But the risk isn’t worth it if you’re on any prescription drug.
There are safer, proven options: therapy, exercise, FDA-approved antidepressants with known safety profiles. You don’t need to gamble with your life for a supplement that’s not regulated, not standardized, and not safe.
If you’re considering it - don’t. If you’re already using it - talk to your provider today. Your meds, your health, and maybe your life depend on it.
Can I take St. John’s Wort with my antidepressant?
No. Combining St. John’s Wort with SSRIs, SNRIs, or other antidepressants can cause serotonin syndrome - a potentially fatal condition. Symptoms include high fever, rapid heart rate, confusion, muscle rigidity, and seizures. Six documented cases in Australia involved patients on citalopram, fluoxetine, or nefazodone. Do not mix them under any circumstances.
How long after stopping St. John’s Wort is it safe to start a new medication?
Wait at least two weeks. The enzyme-inducing effects of hyperforin can linger for up to 14 days after you stop taking St. John’s Wort. If you restart a drug like warfarin, cyclosporine, or an antidepressant too soon, you risk overdose. Always check with your doctor before restarting any medication.
Does St. John’s Wort affect birth control?
Yes. It reduces ethinyl estradiol levels by 25-35%, which can lead to contraceptive failure. There are at least 13 documented cases of unplanned pregnancies in women using birth control pills perfectly while also taking St. John’s Wort. If you’re on hormonal contraception, avoid this herb entirely.
Is St. John’s Wort safe if I only take it occasionally?
No. Even short-term use can trigger interactions. One patient took it for just five days and saw their cyclosporine levels drop 30%. Enzyme induction starts within days. There’s no safe “occasional” use if you’re on prescription drugs.
What should I tell my pharmacist about St. John’s Wort?
Say exactly: “I take St. John’s Wort for depression.” Don’t call it a supplement or herb. Pharmacists are trained to flag drug interactions - but they can’t help if you don’t name it clearly. Bring the bottle or the label. Ask them to check it against all your current prescriptions.
Are there any herbs that are safer than St. John’s Wort for depression?
There’s no herbal supplement proven safe and effective for depression that doesn’t carry interaction risks. Omega-3 fatty acids, exercise, and cognitive behavioral therapy have strong evidence and no known drug interactions. If you’re looking for alternatives, talk to your doctor about these options instead.

Michael Robinson
December 8 2025It’s not about natural vs synthetic. It’s about your body not knowing the difference. A molecule is a molecule. If it changes how your liver works, it’s medicine, no matter what the bottle says.