Difficulty urinating is an uncomfortable and sometimes urgent problem. If you're straining, going slow, or feeling like you can't fully empty your bladder, read this. I'll explain common causes, simple self-checks, and clear signs you need medical help.
First, ask: is the issue sudden or gradual? Sudden inability to pee can be an emergency. Gradual changes often point to long-term issues like prostate growth or bladder muscle weakness. Track how long symptoms have lasted and whether pain, fever, or blood in urine are present.
For men over 50, an enlarged prostate is a leading cause. The prostate can press on the urethra and slow flow. For younger men, infections like prostatitis or urethritis are common. Women may have urinary tract infections, pelvic organ prolapse, or weakened pelvic floor muscles. Other causes that affect anyone include medications (anticholinergics, some antihistamines, opioids), neurological conditions (stroke, diabetes neuropathy, multiple sclerosis), and bladder stones or tumors.
Try these quick checks: note your pee stream (weak, intermittent, or spraying), measure how often you're going and whether you feel the urge but can’t start. Use a diary for 24-48 hours: record fluid intake, number of pees, and if leakage occurs. Try double voiding—after you finish, wait a minute, relax, then try again to see if more urine comes out. Avoid caffeine and alcohol for a day, since they can irritate the bladder.
Over-the-counter remedies rarely fix the root cause, but a warm bath and gentle belly massage can help if retention is from muscle tension. If you're on medication, check labels and talk to your prescriber before stopping anything.
When to call a doctor? If you suddenly can't urinate at all, have severe lower belly pain, fever, vomiting, or blood in urine, seek immediate care. If symptoms persist more than 48 hours, or you notice weight loss, night sweats, or unexplained fatigue alongside urinary changes, schedule an appointment. Bring your pee diary and a list of medications; that speeds diagnosis.
What doctors will do. Expect a physical exam, urine test for infection or blood, and possibly a bladder scan to measure leftover urine. Men may get a prostate exam. Depending on findings, doctors might prescribe antibiotics, adjust medications, recommend a catheter to relieve retention, or refer you for imaging or urology tests like cystoscopy or ultrasound.
Simple lifestyle changes often help: stay hydrated but avoid fluid overload before bedtime, practice pelvic floor exercises, and manage constipation which can press on the bladder. For chronic problems, targeted treatments—medications for prostate size, intermittent self-catheterization, or surgery—can restore normal urination.
Helpful tip: take photos of any urine changes (color, cloudiness) and note new medications or supplements before your visit and dates.
Don't ignore the issue. Difficulty urinating can be temporary or signal a serious condition. If you're unsure, contact your healthcare provider and describe your symptoms clearly. Getting checked early prevents complications and gets you back to normal faster.
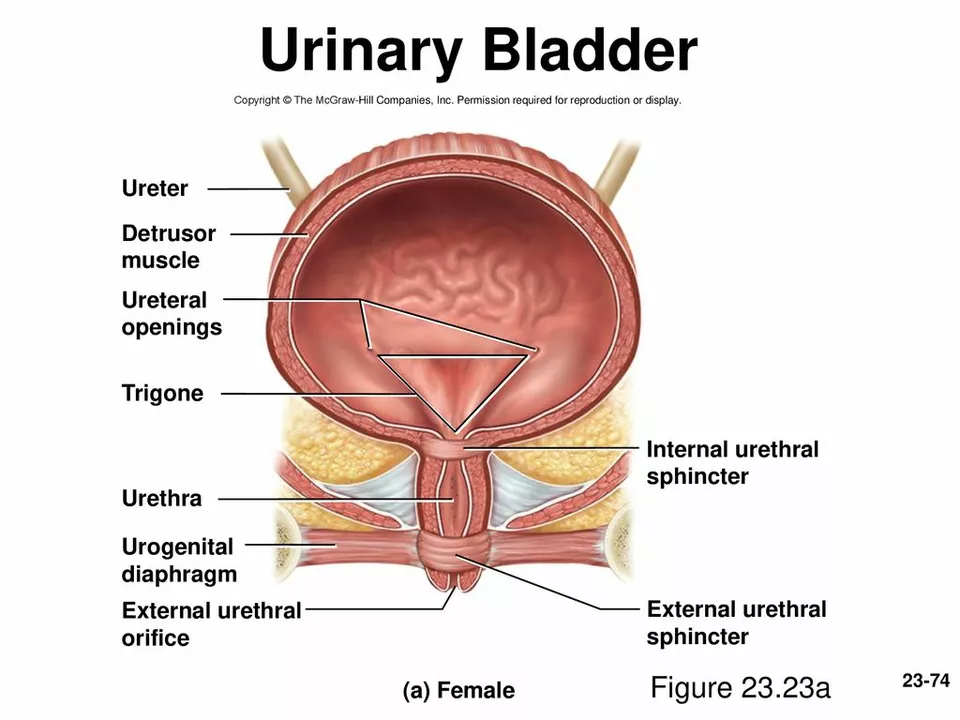
As someone who has been researching bladder health, I recently discovered the connection between bladder prolapse and difficulty urinating. Bladder prolapse, also known as cystocele, occurs when the bladder's supportive tissue weakens, causing it to drop and press against the vaginal wall. This can lead to difficulty urinating, as the bladder's position and function may be compromised. In some cases, this may result in incomplete emptying of the bladder and an increased risk of urinary tract infections. It's important to be aware of this connection and seek medical advice if you're experiencing any difficulty urinating or other related symptoms.