When talking about Contraceptive Effectiveness, the measure of how well a birth‑control method prevents pregnancy when used correctly. Also known as birth control success rate, it tells you how many users will stay pregnancy‑free over a year of typical use. Understanding this metric helps you compare pills, patches, IUDs, condoms, and more, so you can pick a method that fits your lifestyle and health profile.
One of the biggest players in the effectiveness game is Hormonal Contraception, methods that use synthetic estrogen, progestin, or both to stop ovulation. These include combined oral pills, the patch, the vaginal ring, and hormonal IUDs. Because they control hormone levels, they typically boast perfect‑use failure rates below 1 %. However, typical‑use rates rise a bit due to missed pills or delayed patch changes, showing how user behavior directly impacts outcomes.
Speaking of devices, the Intrauterine Device (IUD), a small, T‑shaped implant placed in the uterus is another top performer. Copper IUDs and hormonal IUDs both achieve less than 1 % failure with typical use because once placed, there’s little you can do wrong. The key trade‑off is a minor procedure and, for copper IUDs, a slightly higher risk of heavier periods.
On the other end of the spectrum are Barrier Methods, physical blocks like condoms, diaphragms, and cervical caps. These rely entirely on correct and consistent use each time you have sex. Perfect‑use failure rates can be under 2 %, but typical use often jumps to 13‑18 % because of slippage, breakage, or forgetting to apply them.
Another often‑overlooked factor is User Adherence, how faithfully a person follows the method’s instructions. Studies show that adherence is the single biggest predictor of real‑world effectiveness. Missed pills, delayed injections, or inconsistent condom use all widen the gap between perfect and typical use.
Health risks also shape method choice. For example, certain hormonal pills raise the risk of blood clots, especially in smokers or women over 35. If clot risk is a concern, a copper IUD or a progestin‑only option may be safer. This illustrates the semantic triple: Risk factors such as blood clot propensity influence contraceptive effectiveness outcomes.
Cost and access matter, too. Over‑the‑counter condoms are cheap but have higher typical‑use failure, while prescription methods like IUDs have higher upfront costs but lower long‑term failure. Your budget can therefore affect the overall effectiveness you experience.
In short, contraceptive effectiveness isn’t just a number – it’s a blend of method type, how you use it, your health profile, and practical considerations like cost. Knowing the typical‑use and perfect‑use rates helps you set realistic expectations and choose a method that aligns with your daily routine.
Below you’ll find a collection of articles that dive deeper into related health topics – from blood‑clot risk and heart health to hormone interactions and lifestyle tips – giving you a fuller picture of how the right birth‑control choice fits into overall well‑being.
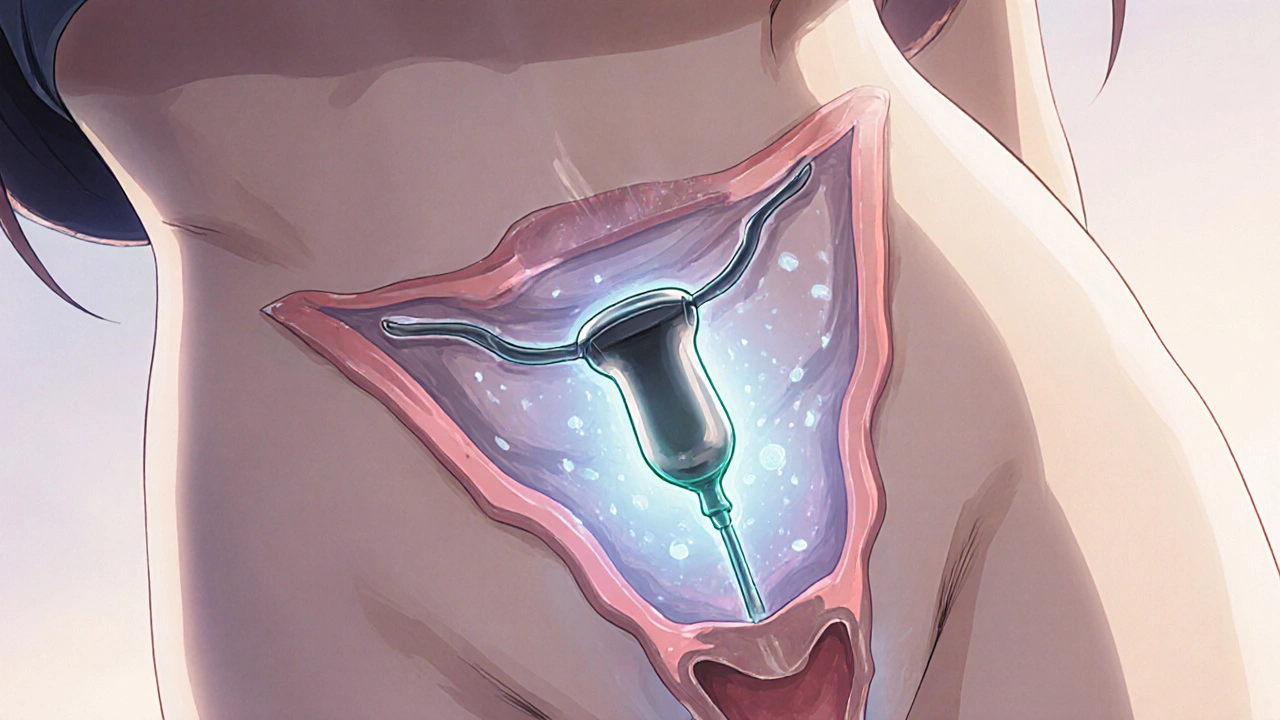
Explore the benefits, side effects, costs, and suitability of levonorgestrel-releasing intrauterine devices, with clear pros‑cons and practical guidance for choosing this hormonal IUD.