Levonorgestrel IUD Comparison Tool
Compare Your Options
Birth Control Method Comparison
Based on your selections, here's how levonorgestrel IUD compares to other methods:
| Method | Effectiveness | Duration | Key Benefits | Potential Drawbacks |
|---|---|---|---|---|
| Levonorgestrel IUD | 0.2% typical-use failure rate (Highly effective) |
3-7 years | - Reduces menstrual bleeding (up to 80%) - Fertility returns quickly (within 6 weeks) - No daily maintenance required | - Initial irregular bleeding (3-6 months) - Insertion discomfort - Hormonal side effects possible |
| Oral Contraceptives | 7-9% typical-use failure rate (Less effective) |
30 days | - Adjustable - Can regulate periods | - Must be taken daily - Side effects like nausea, headaches |
| Copper IUD | 0.8% typical-use failure rate (Highly effective) |
10 years | - Hormone-free - Long-lasting - Emergency contraception | - Heavier, more painful periods - Higher expulsion risk |
| Hormonal Implant | 0.05% typical-use failure rate (Extremely effective) |
3 years | - Very effective - No daily maintenance - Can reduce bleeding | - Irregular bleeding - Hormonal side effects |
Important Note
Individual experiences with birth control vary. This comparison is based on statistical averages from clinical studies. Always discuss your options with a healthcare provider to determine what's best for your personal health needs.
When you hear the term levonorgestrel-releasing intrauterine device is a small, T‑shaped device that sits inside the uterus and slowly releases the synthetic hormone levonorgestrel, you probably think of a high‑tech birth control method. It’s actually a straightforward, long‑lasting option that millions of people rely on every day. Below we break down why the levonorgestrel IUD is praised, where it can fall short, and what you should weigh before deciding if it matches your lifestyle.
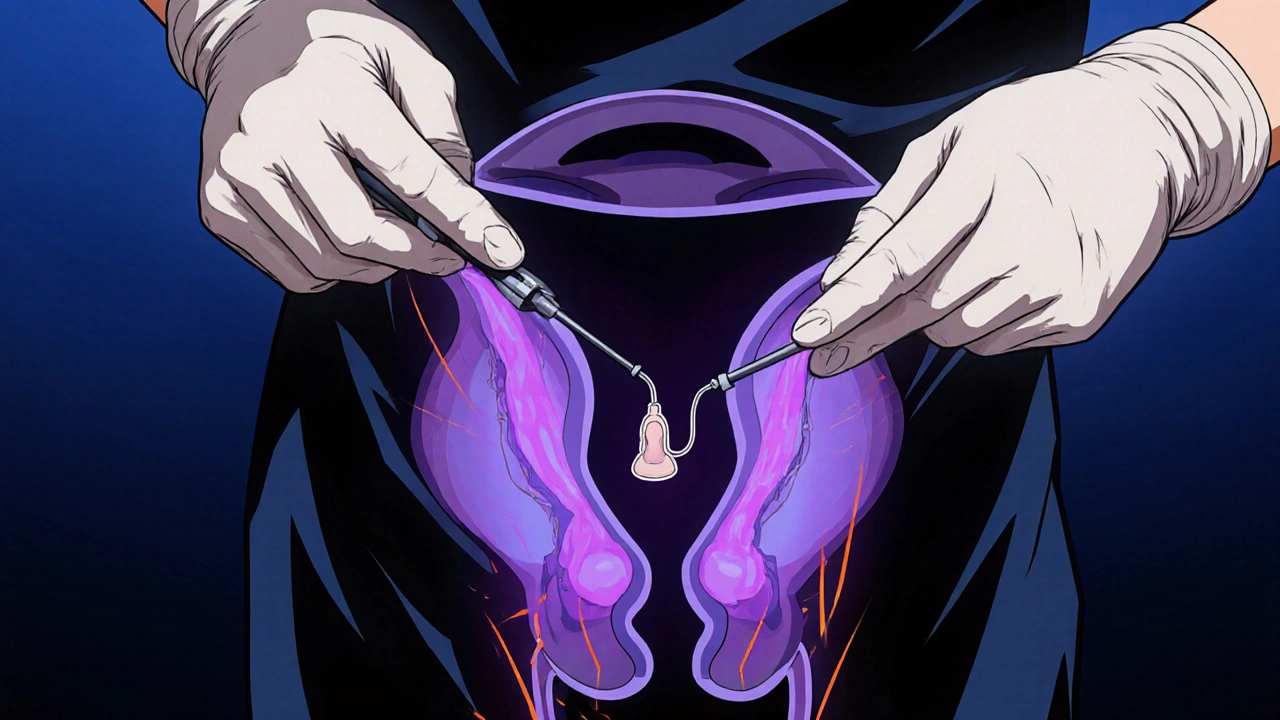
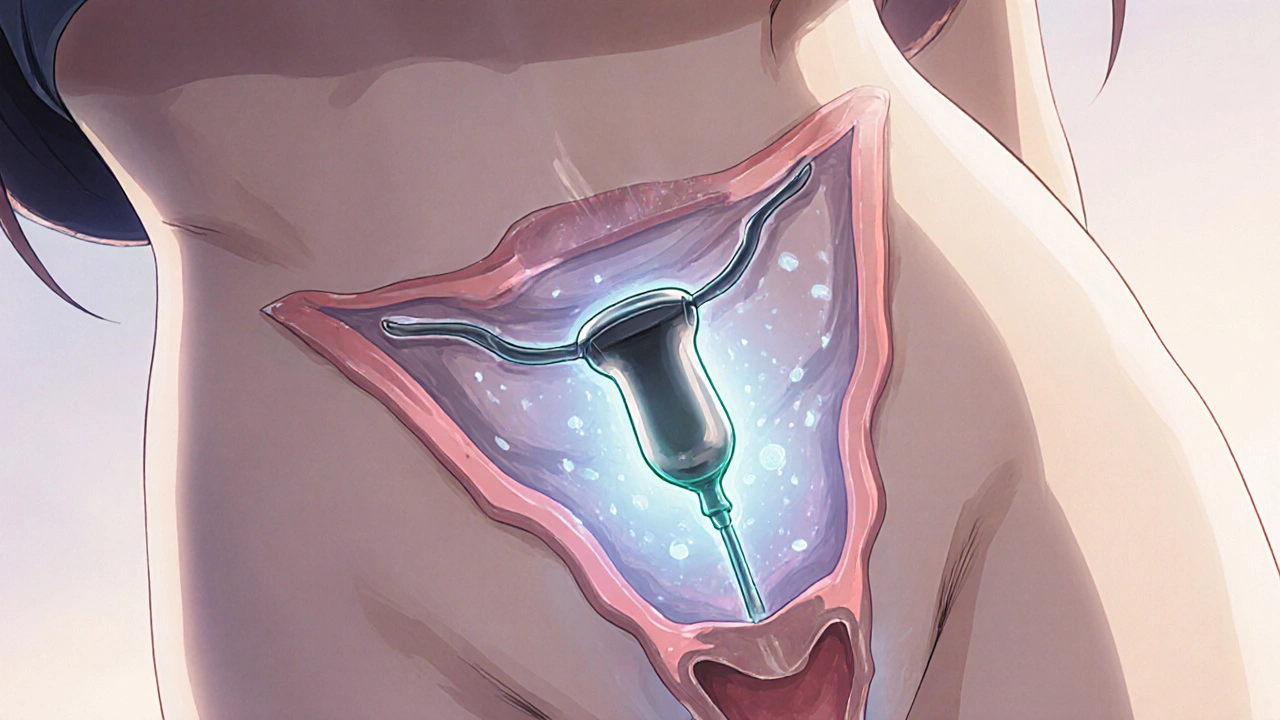
How the LNG‑IUD Works
The device releases a tiny amount of levonorgestrel (about 20 µg per day at start, tapering to 10 µg after a year). This hormone thickens cervical mucus, thins the uterine lining, and can suppress ovulation in some users. The result is a highly effective barrier against sperm while also making periods lighter or even stopping them altogether.
Effectiveness Compared to Other Methods
In real‑world studies, the typical‑use failure rate for LNG‑IUDs sits at 0.2 %-the same ballpark as sterilization and far better than pills, patches, or rings, which hover around 7‑9 %. The copper intrauterine device (Cu‑IUD) is similarly effective, but the hormonal option adds menstrual benefits.
Advantages of Levonorgestrel IUDs
- Long‑term protection: most devices stay in place for 3‑7 years, depending on the brand.
- Reduced menstrual bleeding: up to 80 % of users experience lighter periods; about 20 % stop bleeding entirely after 6 months.
- Convenient: after insertion you don’t need to remember a daily pill.
- Fertility returns quickly: ovulation typically resumes within 6 weeks after removal.
- Non‑contraceptive health gains: lower risk of endometrial hyperplasia and a modest reduction in ovarian cysts.
Potential Disadvantages and Side Effects
- Irregular bleeding during the first 3-6 months is common; some users report spotting or breakthrough bleeding.
- Insertion discomfort - a brief cramp or pinching feeling is normal, but severe pain may indicate a problem.
- Hormonal side effects such as breast tenderness, mood swings, or acne can appear, especially during the first cycle.
- Risk of expulsion: about 2‑5 % of users experience the device slipping out, often after vigorous activity or postpartum.
- Rare complications like perforation (<0.1 %) or pelvic inflammatory disease (PID) in the first 20 days if an existing infection is present.
Comparing Brands: Mirena, Kyleena, Skyla, Liletta
| Brand | Size (mm) | Hormone release (µg/day) | Approved duration | Typical price (AUD) |
|---|---|---|---|---|
| Miranda (formerly Mirena) | 32 × 32 | 20 → 10 | 5 years | ≈ $215 |
| Kyleena | 28 × 30 | 17.5 → 7.5 | 5 years | ≈ $190 |
| Skyla | 28 × 30 | 14 → 6 | 3 years | ≈ $180 |
| Liletta | 32 × 32 | 20 → 10 | 6 years | ≈ $200 |
Who Benefits Most From a Levonorgestrel IUD?
People who want a set‑and‑forget method and dislike monthly pills are obvious candidates. It shines for those with heavy or painful periods-up to nine in ten report a big cut in bleeding after a year. Women with a history of endometrial hyperplasia or who want to reduce ovarian cyst risk also gain a hormonal edge over copper IUDs.
When an LNG‑IUD Might Not Be the Right Choice
If you are pregnant, have active pelvic infection, or have uterine anomalies (like a large fibroid), a hormonal IUD could be unsafe. Those who experience severe mood changes on hormonal contraception should discuss alternatives with a clinician. Finally, people who prefer a hormone‑free method might lean toward copper IUDs despite the downside of heavier periods.
Insertion, Removal, and Follow‑Up
- Schedule a brief appointment with a trained clinician. A pelvic exam confirms size and positioning.
- The provider inserts the IUD through the cervix using a thin applicator. The process usually takes 5-10 minutes.
- After insertion, you’ll be asked to check the strings monthly for placement.
- When you decide to stop, the provider removes the device in a similar quick office visit.
Most users report mild cramping for a day or two after both insertion and removal-over‑the‑counter ibuprofen works well.
Cost, Insurance, and Access in Australia (2025)
Under the Australian Pharmaceutical Benefits Scheme (PBS), the LNG‑IUD is subsidized for most eligible patients, bringing the out‑of‑pocket cost down to about $30‑$50. Private clinics charge a higher fee that includes insertion; these can range from $150 to $250. Many health insurers reimburse the full amount when a doctor’s referral is provided.
Quick Checklist Before You Decide
- Do you want long‑term, low‑maintenance contraception?
- Are you comfortable with a small amount of hormone each month?
- Do you have any current pelvic infection or uterine abnormalities?
- Is reducing menstrual bleeding a priority for you?
- Can you afford the upfront cost or access PBS subsidies?
If you answered “yes” to most of these, the levonorgestrel IUD is worth a deeper conversation with your health professional.
Common Myths Debunked
Myth: The IUD can cause infertility.
**Fact:** Fertility returns quickly after removal; studies show no long‑term impact on the ability to conceive.
Myth: Hormonal IUDs increase cancer risk.
**Fact:** Levonorgestrel actually lowers the risk of endometrial cancer and does not raise breast cancer rates.
Myth: You need a partner’s consent to use an IUD.
**Fact:** In Australia, adults can decide independently; minors may need parental consent depending on state laws.
Frequently Asked Questions
How long does a levonorgestrel IUD protect against pregnancy?
Depending on the brand, protection lasts between 3 and 7 years. The device can be removed at any time without affecting future fertility.
Will the IUD make my periods stop completely?
Many users experience lighter periods or no bleeding after six months. A small proportion continue to have regular cycles.
Can I use an LNG‑IUD while breastfeeding?
Yes. Hormonal IUDs are considered safe for lactating mothers and do not affect milk production.
What should I do if I feel the IUD strings longer than usual?
Contact your clinician. Occasionally the strings can coil higher in the cervix, but a quick exam will confirm proper placement.
Is the LNG‑IUD covered by Medicare?
Under the PBS, most eligible patients pay a reduced fee. Private health funds often cover the full cost when a doctor’s prescription is provided.
Choosing the right contraceptive method is personal, but the levonorgestrel‑releasing IUD offers a blend of high effectiveness, menstrual benefits, and convenience that few other options match. Talk with a trusted health professional, weigh the pros and cons listed here, and decide what fits your life best.

Poornima Ganesan
October 18 2025Let’s start with the basics: the levonorgestrel IUD is not a futuristic gadget, it’s a proven, hormone‑releasing device that has been around for decades.
It works by delivering a steady micro‑dose of levonorgestrum directly into the uterine cavity, which means systemic exposure is minimal compared to oral contraceptives.
The hormone thickens cervical mucus, thins the endometrial lining, and-yes, in some cases-suppresses ovulation, creating a multi‑layered barrier against conception.
Effectiveness numbers are astonishing: a 0.2 % failure rate puts it on par with sterilisation, which is why many clinicians rank it at the top of the contraceptive hierarchy.
The menstrual benefits are often under‑emphasised; up to 80 % of users report lighter periods and about 20 % stop bleeding altogether after six months.
This can be a game‑changer for people with menorrhagia or anemia, yet the literature rarely mentions the quality‑of‑life improvements in a systematic way.
Insertion discomfort is a reality-there is a brief cramp, a pinch, perhaps even a faint feeling of pressure-but serious pain is the exception, not the rule.
Speaking of exceptions, the risk of expulsion (2‑5 %) and perforation (approximately 1 in 1,000) are real, albeit low, complications that should be discussed transparently before the procedure.
Hormonal side‑effects such as breast tenderness, mood swings, or acne tend to surface in the first cycle, but they usually attenuate over time as the body adapts.
What often goes unnoticed is the non‑contraceptive benefit: a modest reduction in the incidence of ovarian cysts and a lowered risk of endometrial hyperplasia.
On the flip side, irregular spotting in the initial three‑to‑six months is common, and patients sometimes misinterpret this as treatment failure.
Because the device releases roughly 20 µg of levonorgestrel per day initially, tapering to about 10 µg after a year, the hormone load is substantially lower than that of many oral formulations.
That said, the systemic hormone exposure, although limited, can still influence mood and libido, and clinicians should monitor these variables closely.
Another point of contention is the cost: while the upfront price may seem steep, the cumulative expense over a decade often undercuts that of monthly pills, especially when insurance coverage is factored in.
In summary, the levonorgestrel IUD offers a blend of high efficacy, menstrual management, and convenience, but it is not without its caveats-especially regarding insertion pain, early bleeding irregularities, and the rare but serious risks of perforation and expulsion.