Seeing two health things described as “connected” can be alarming. You might read that ulcerative colitis raises colon cancer risk or that a rare tumor can mess with blood sugar. This tag collects plain‑spoken articles that dig into those links and tell you what they actually mean — not alarmist headlines.
We cover different kinds of connections: disease-to-disease links, drug interactions, how one medication affects another condition, and even links between online pharmacy practices and safety. Each post tries to show the evidence, how strong it is, and the practical takeaway for you.
Start by asking three simple questions: What kind of study is this (case report, cohort, randomized trial)? How big is the effect (a tiny increase in risk vs a large one)? And is the result recent and repeated by others? A single small study can hint at a link, but repeated research and clear biological reasons make it more believable.
Look for whether authors report absolute numbers. Hearing “risk doubles” sounds scary, but if the original risk was 1 in 10,000 and it becomes 2 in 10,000, the real change is small. Also check whether the study controlled for other factors — age, smoking, weight — because those often explain apparent links.
Don’t panic. Use articles as a starting point, not a diagnosis. Write down the main points and any numbers you don’t understand, then ask your clinician specific questions: Do I need extra screening? Should my meds change? Is this risk relevant given my age and history? If you’re on medication, never stop or switch doses without a doctor’s okay.
If the article suggests an urgent risk — new severe symptoms, sudden blood sugar changes, major allergic signs — seek medical care right away. For longer‑term concerns (cancer screening, chronic condition management), ask for a plan you can follow: which tests, how often, and what lifestyle steps help reduce risk.
Use this tag page to find focused reads: examples include pieces on ulcerative colitis and colon cancer, pheochromocytoma and diabetes, and practical guides about drug interactions like Fluconazole and alcohol. Each post links to sources so you can read the studies yourself if you want.
Quick checklist before acting:
If you want help understanding a specific article from this tag, paste the headline or link and I’ll pull out the key points and practical steps you can take next.
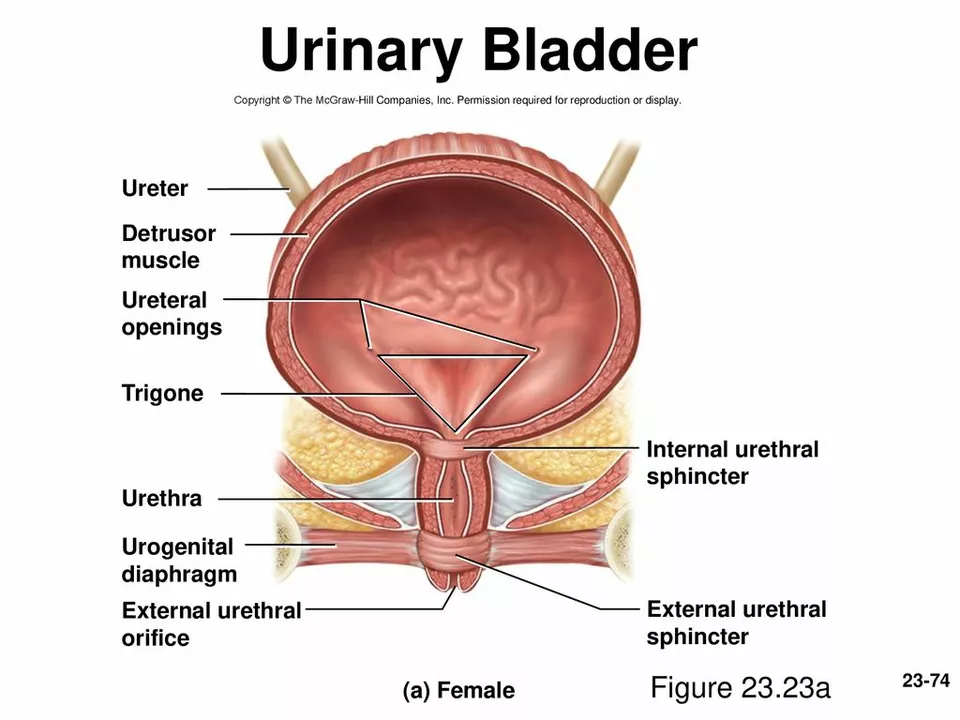
As someone who has been researching bladder health, I recently discovered the connection between bladder prolapse and difficulty urinating. Bladder prolapse, also known as cystocele, occurs when the bladder's supportive tissue weakens, causing it to drop and press against the vaginal wall. This can lead to difficulty urinating, as the bladder's position and function may be compromised. In some cases, this may result in incomplete emptying of the bladder and an increased risk of urinary tract infections. It's important to be aware of this connection and seek medical advice if you're experiencing any difficulty urinating or other related symptoms.