When your liver is scarred from cirrhosis, a late-stage liver disease where healthy tissue is replaced by scar tissue, impairing function. It's not just about medication—it's about what you put on your plate. A cirrhosis diet isn’t a fad. It’s a practical, evidence-backed way to reduce pressure on your liver, control fluid buildup, and prevent confusion caused by toxin buildup. This isn’t about starving yourself or eating bland food. It’s about making smart choices that give your body the support it needs while avoiding triggers that make things worse.
One of the biggest problems in cirrhosis is ascites, fluid buildup in the abdomen that causes swelling, discomfort, and breathing trouble. The main culprit? Too much sodium. Most people don’t realize how much salt is hiding in bread, canned soups, deli meats, and even breakfast cereals. Cutting sodium isn’t just a suggestion—it’s often the difference between going home from the hospital and being readmitted. Most doctors recommend under 2,000 mg a day. That means reading labels, cooking at home, and saying no to restaurant meals unless you know exactly what’s in them.
Another key piece is protein, essential for muscle repair and preventing muscle wasting, which is common in advanced liver disease. For years, doctors told cirrhosis patients to limit protein because of concerns about confusion (hepatic encephalopathy). But newer research shows that too little protein makes things worse. The trick? Choose high-quality sources like eggs, lean poultry, fish, tofu, and low-fat dairy. Avoid processed meats. And spread your protein evenly across meals instead of loading it all into dinner.
Then there’s fluid intake, which may need to be limited if you have severe ascites or low sodium levels. This isn’t about drinking less water because you’re thirsty—it’s about balancing what your body can handle. If your doctor says to limit fluids, they’ll give you a specific number. Don’t guess. And don’t assume all fluids are the same. Coffee, tea, and broth count too.
Alcohol? Absolutely off-limits. No exceptions. Even small amounts can keep damaging your liver. And while you’re at it, skip supplements unless your doctor approves them. Some herbs, vitamins, and weight-loss products can be toxic to a liver already under stress. Same goes for over-the-counter painkillers like ibuprofen or naproxen—they can hurt your kidneys, which are already working harder because of cirrhosis.
What about fruits and vegetables? Eat them. They’re full of fiber, antioxidants, and nutrients your liver needs to function better. But wash them well. Your immune system is weaker, so you’re more vulnerable to foodborne illness. Avoid raw shellfish—it can carry bacteria that cause dangerous infections in people with liver disease.
There’s no magic food that fixes cirrhosis. But the right diet slows decline, reduces hospital visits, and gives you more energy to do the things you love. The posts below cover real-life strategies: how to read food labels when you’re tired, what to do when you lose your appetite, how to handle cravings without breaking your diet, and why some supplements that sound helpful can actually be dangerous. These aren’t theory pages—they’re practical tools from people who’ve been there.
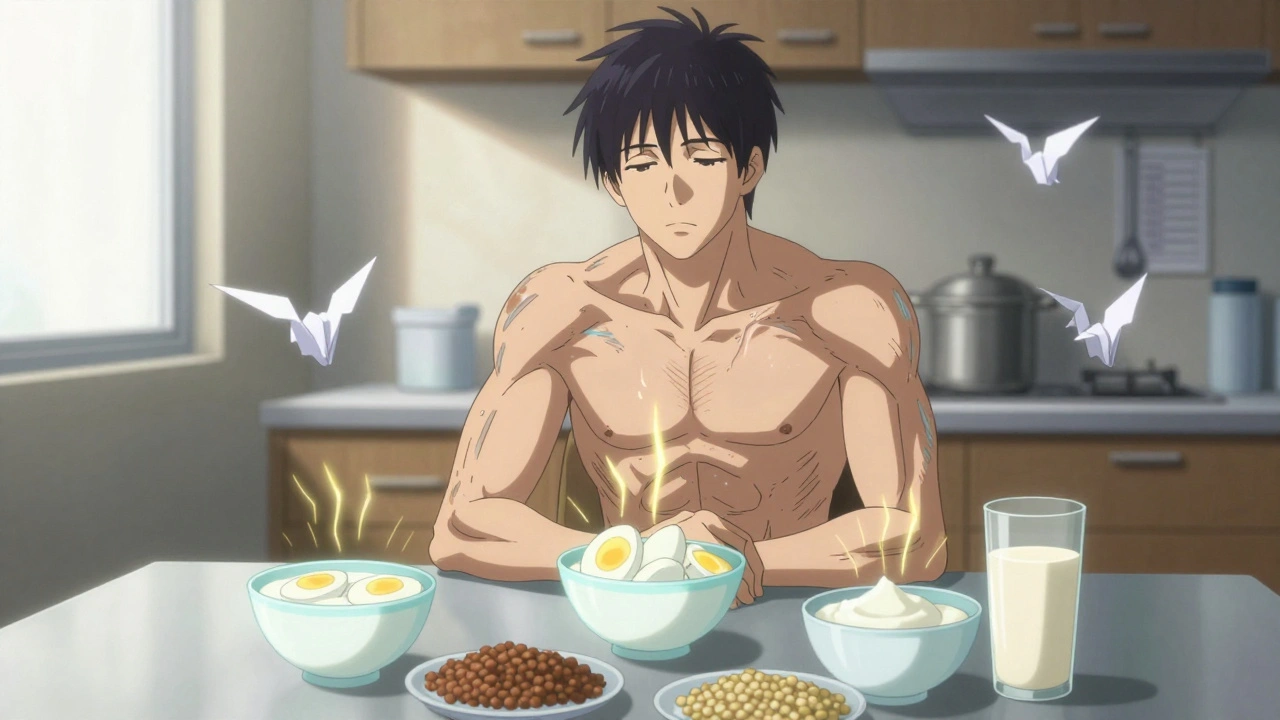
Learn how proper protein intake helps preserve muscle, reduce complications, and improve survival in cirrhosis. Stop outdated myths and follow science-backed nutrition guidelines.