For years, people with cirrhosis were told to cut back on protein. The idea was simple: less protein means less ammonia, and less ammonia means fewer brain fog episodes. But that advice, once common in clinics and hospitals, is now outdated-and potentially dangerous. Today, we know that protein isn’t the enemy. In fact, not getting enough of it can speed up muscle loss, weaken your body, and even shorten your life.
Why Protein Matters More Than Ever in Cirrhosis
Cirrhosis isn’t just a damaged liver. It’s a full-body metabolic crisis. Your body is stuck in a constant state of breakdown. Muscles are being eaten away for energy, even when you’re resting. This isn’t normal aging. It’s called sarcopenia, and it affects between 40% and 70% of people with cirrhosis. Studies show that those with muscle loss are two to three times more likely to die, whether they’re waiting for a transplant or managing the disease at home. The old thinking was that protein caused hepatic encephalopathy (HE)-the confusion, memory problems, and slurred speech linked to liver failure. But research from 2004 changed everything. In a controlled trial, patients on a normal protein diet (1.2 grams per kilogram of body weight) didn’t have worse HE than those on a low-protein diet (0.5 grams per kilogram). Instead, the low-protein group lost muscle faster. Their bodies started breaking down their own tissue just to survive. Today, the American Association for the Study of Liver Diseases (AASLD), the European Association for the Study of the Liver, and other top liver groups all agree: protein restriction does more harm than good. You need protein-not to avoid brain fog, but to stop your body from eating itself.How Much Protein Do You Really Need?
The numbers might surprise you. Most experts recommend 1.2 to 1.5 grams of protein per kilogram of your dry body weight per day. Dry weight means your weight without extra fluid-because cirrhosis causes fluid buildup in the belly and legs, which can make you look heavier than you actually are. For example, if your dry weight is 70 kilograms (about 154 pounds), you need 84 to 105 grams of protein daily. That’s not a huge amount, but it’s hard to hit if you’re eating small meals due to bloating or loss of appetite. If you’re already losing muscle, aim for the higher end: 1.5 grams per kilogram. If you’re very sick or hospitalized, you may need up to 2.0 grams per kilogram. Your doctor or dietitian can help you figure out your exact number. Don’t rely on your scale. Fluid retention masks real weight. Ask your care team to estimate your dry weight using body composition tools or clinical signs like reduced swelling after diuretics.Best Protein Sources for Cirrhosis
Not all protein is created equal. Animal proteins like beef, chicken, and fish are high in protein-but they can be harder to digest and may trigger HE in some people. Plant and dairy proteins are better tolerated and often recommended. Here’s what to focus on:- Dairy: Milk, yogurt, cottage cheese, low-salt cheese. One cup of milk has about 8 grams of protein.
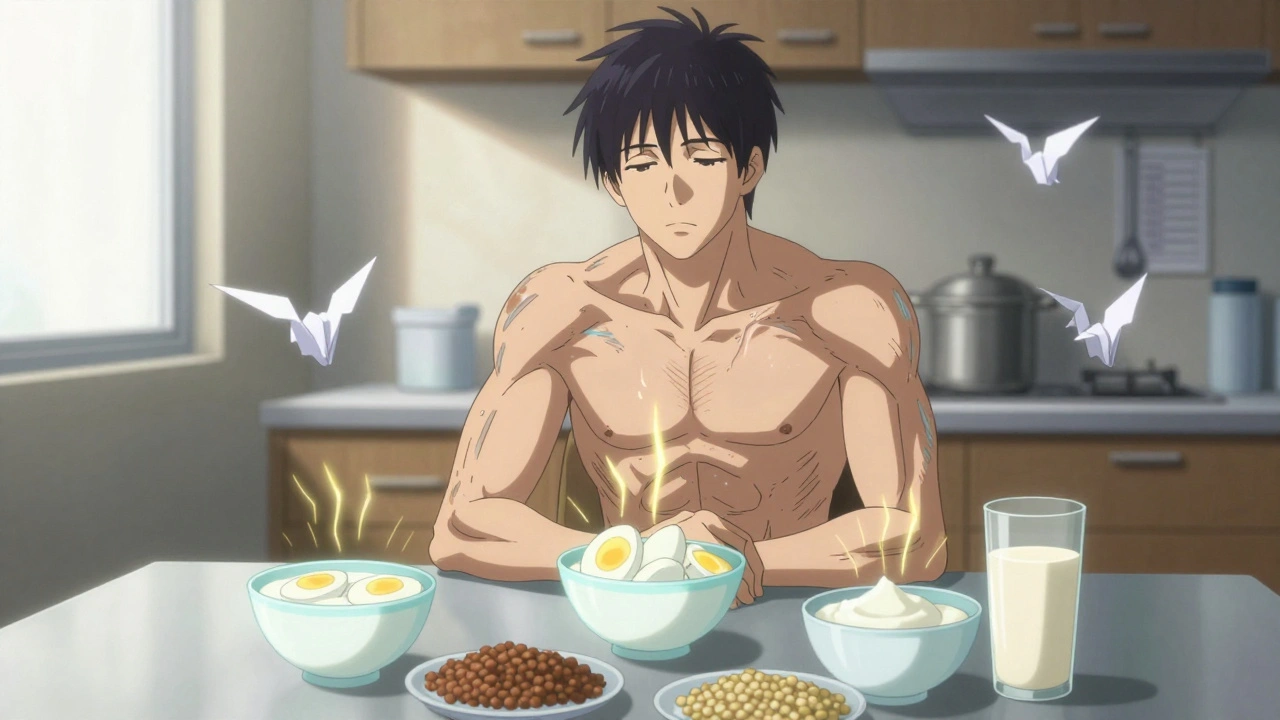
- Eggs: One large egg has 6 grams. Easy to eat, easy to digest.
- Plant-based: Lentils, beans, tofu, edamame, soy milk, nuts, oats, wild rice. These are gentle on the liver and rich in fiber.
- Protein supplements: If you can’t eat enough, your doctor may prescribe a high-protein shake. Look for ones with whey or plant-based protein and no added sugar.

Meal Timing: Why Snacking Matters
Eating three big meals a day won’t cut it. Your body needs steady fuel. Going more than 4 hours without eating triggers muscle breakdown. Overnight fasting is especially harmful. The solution? Eat every 2 to 4 hours while you’re awake. That means 5 to 6 small meals or snacks a day. One critical habit: a late-night protein snack. Have something with 15 to 20 grams of protein about 1 to 2 hours before bed. Examples:- 1 cup of Greek yogurt
- 2 hard-boiled eggs
- 1 scoop of protein powder mixed with water
- Half a cup of cottage cheese with a few almonds
Calories Are Just as Important as Protein
You can’t build muscle if you’re not eating enough total calories. Your body will use protein for energy instead of rebuilding tissue. That defeats the whole purpose. AASLD recommends at least 35 calories per kilogram of dry weight per day if your BMI is normal. If you’re overweight, you still need 25-35 calories per kilogram. If you’re severely overweight (BMI over 40), aim for 20-25 calories per kilogram. To get enough calories without feeling full:- Choose whole milk over skim milk
- Add butter or olive oil to vegetables and grains
- Snack on dried fruit, nuts, or avocado
- Use full-fat yogurt and cheese
What About Sodium and Fluids?
Many people with cirrhosis are told to cut salt to reduce swelling. But if you’re struggling to eat enough, being too strict with sodium can backfire. If you’re losing weight or can’t meet your protein goals, your doctor may allow slightly more salt to help you eat more. Don’t cut fluids unless you’re told to. Dehydration makes muscle loss worse. Drink water, broth, or oral rehydration solutions if you’re losing fluids from diuretics.
Micronutrients You Might Be Missing
Cirrhosis messes with how your body absorbs and uses vitamins and minerals. Common deficiencies include:- Zinc: Helps with taste, appetite, and healing. Doctors often prescribe 50 mg daily.
- Thiamine (B1), Niacin (B3), Pyridoxine (B6), Folate: Support energy and nerve function.
- Magnesium: Needed for muscle function and protein synthesis.
What If You Can’t Eat Enough?
Loss of appetite, early fullness, nausea, and taste changes are common. That’s normal. But it’s not okay to go without enough protein. Solutions:- Try high-protein snacks: Nature Valley Protein bars (40g protein), Clif Builder’s Bars (68g protein), or protein shakes.
- Use nutritional supplements prescribed by your doctor-these are specially made for liver patients.
- Blend meals into smoothies: Greek yogurt, banana, peanut butter, and protein powder can be easier to swallow than solid food.
- Work with a registered dietitian who understands liver disease. They can create a personalized plan.
The Big Picture: Protein Is Your Lifeline
This isn’t about eating more steak. It’s about protecting your body from the inside out. Every gram of protein you get helps your muscles stay strong, your immune system work, and your liver handle stress. It’s not a luxury-it’s survival. The outdated idea that protein causes brain fog has been debunked. The real danger is not eating enough. If you’ve been told to cut protein, talk to your doctor. Ask for a referral to a dietitian who specializes in liver disease. Get your dry weight checked. Track your meals. Add a bedtime snack. Your body is fighting hard. Give it the tools to fight back.Should I avoid protein if I have hepatic encephalopathy?
No. Avoiding protein does not improve hepatic encephalopathy and can make muscle loss worse. Current guidelines from the American Association for the Study of Liver Diseases (AASLD) and other major liver organizations recommend 1.2-1.5 grams of protein per kilogram of dry body weight daily, even for people with HE. Protein from plant and dairy sources is often better tolerated than meat. Focus on lentils, beans, tofu, yogurt, and eggs.
How do I calculate my protein needs if I have fluid retention?
Use your dry body weight-not your current scale weight. Dry weight is your weight after excess fluid is removed, often after diuretics or hospitalization. If you don’t know your dry weight, ask your doctor or dietitian. A general rule is 1.2-1.5 grams of protein per kilogram of dry weight. For example, if your dry weight is 65 kg, aim for 78-98 grams of protein daily. Don’t base your intake on swollen weight-it will lead to under-eating.
Can I get enough protein without eating meat?
Yes. Many people with cirrhosis do better on plant-based and dairy proteins. Good sources include tofu, edamame, lentils, beans, Greek yogurt, cottage cheese, eggs, and soy milk. A cup of lentils has about 18 grams of protein, and a cup of Greek yogurt has 20 grams. Combining these throughout the day easily meets daily targets without meat.
Why is a bedtime snack important?
Overnight fasting causes your body to break down muscle for energy. A high-protein snack 1-2 hours before bed helps prevent this. It improves nitrogen balance and supports muscle repair while you sleep. Good options: 1 cup of cottage cheese, 2 hard-boiled eggs, or a protein shake. This simple habit can make a big difference in preserving strength and function.
What supplements are safe for cirrhosis?
Zinc (50 mg daily) is commonly recommended and well-tolerated. B-complex vitamins and magnesium may help if you’re deficient. Avoid high-dose vitamin A, vitamin D, and vitamin C if you have hemochromatosis. Always talk to your doctor before starting any supplement. Prescription-grade protein shakes are often safer than over-the-counter ones because they’re designed for liver patients and have balanced nutrients.

Tommy Walton
December 2 2025Protein isn't just food-it's biohacking for your liver. 🧬 If you're not hitting 1.5g/kg dry weight, you're basically letting your body cannibalize itself. Stop listening to 2003 guidelines. This isn't nutrition. It's survival engineering.