Why Patient Education Is Critical for Safe Cyclosporine Therapy
Cyclosporine isn’t just another pill. It’s a powerful immunosuppressant that keeps transplanted organs from being rejected - or keeps autoimmune diseases like psoriasis or rheumatoid arthritis under control. But it’s also one of the most dangerous drugs if used wrong. A single missed dose, a glass of grapefruit juice, or an over-the-counter painkiller can send blood levels soaring or crashing. And when that happens, patients don’t just feel unwell - they risk kidney failure, nerve damage, or even organ rejection.
Here’s the hard truth: cyclosporine therapy fails more often because of poor patient understanding than because of the drug itself. Studies show that up to 40% of transplant patients on cyclosporine experience treatment complications linked to non-adherence or misunderstandings about how to take it. That’s not a failure of the medicine. It’s a failure of education.
What Cyclosporine Does - and Why It’s So Tricky
Cyclosporine works by blocking T-cells, the immune system’s soldiers. That’s exactly what you want after a kidney or liver transplant. But it doesn’t pick and choose. It shuts down your whole defense system. That’s why patients on cyclosporine are at higher risk for infections, skin cancers, and high blood pressure.
And here’s what makes it worse: cyclosporine has a very narrow therapeutic window. That means the difference between a safe, effective dose and a toxic one is tiny. Blood levels need to be checked every few weeks - sometimes even weekly - especially when starting treatment or changing doses. But no one can monitor your blood 24/7. That’s where patient education becomes your last line of defense.
The Top Three Mistakes Patients Make With Cyclosporine
Most errors aren’t due to forgetfulness. They’re due to misinformation.
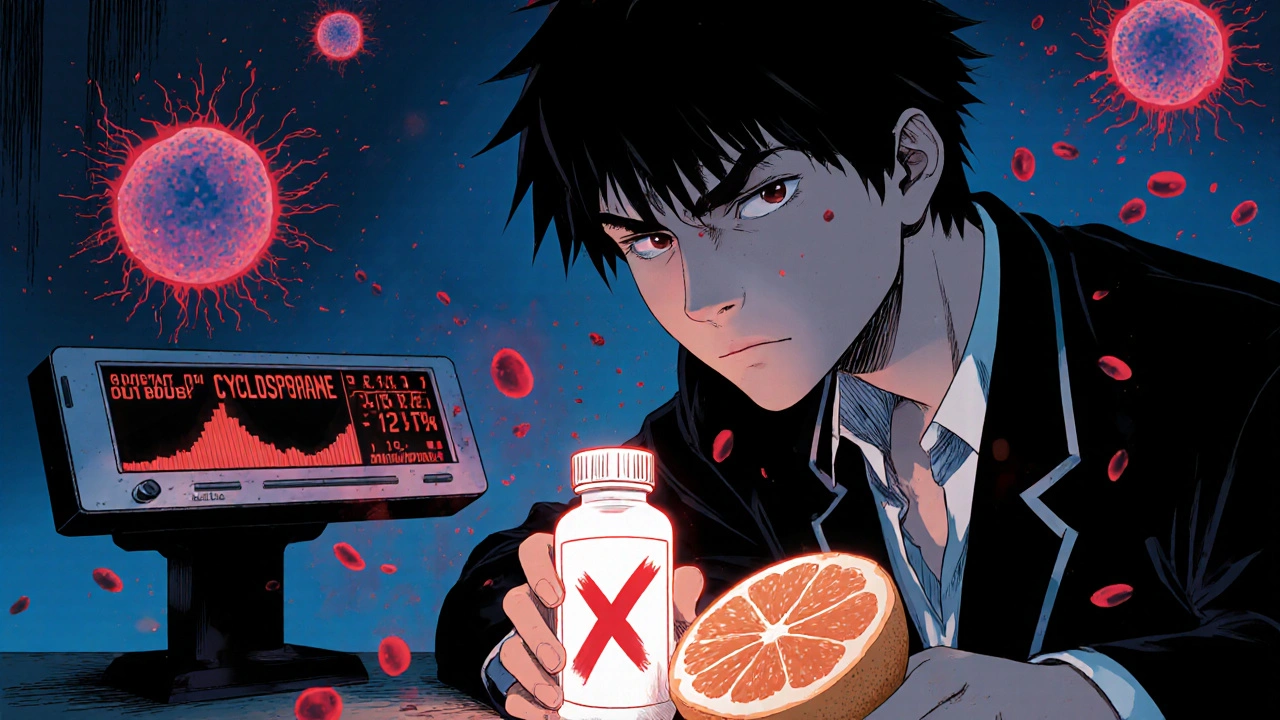
- Taking it with grapefruit or grapefruit juice - This single fruit can raise cyclosporine levels by up to 500%. One glass can push you into toxic range. No exceptions.
- Skipping doses because you feel fine - Cyclosporine doesn’t cause immediate symptoms when levels drop. But rejection can start quietly, inside your new organ. You won’t feel it until it’s too late.
- Using OTC meds like ibuprofen or naproxen - These painkillers stress the kidneys. Cyclosporine already does. Together, they can cause acute kidney injury in days.
One patient in Melbourne, a 52-year-old man who had a liver transplant, stopped taking his cyclosporine for three days because he had a cold and thought he "didn’t need it." He ended up in the ER with signs of rejection. His new liver was saved - but barely. His doctors said it was preventable.
What Good Patient Education Looks Like
Good education isn’t a one-time pamphlet handed out at discharge. It’s ongoing, personalized, and repeated.
- Clear dosing instructions - "Take 300 mg twice a day" isn’t enough. Patients need to know: "Take it at 8 a.m. and 8 p.m., 1 hour before meals, with a full glass of water." Timing matters because food affects absorption.
- Visual aids - A color-coded pill box labeled with times and warnings helps. A picture of grapefruit with a red "X" over it sticks better than a warning label.
- Real-life scenarios - "What if you’re sick and can’t eat?" "What if you miss a dose?" "What if you start a new supplement?" Walk through these situations together.
- Know your blood test numbers - Patients should understand what their cyclosporine trough level means. A level of 150 ng/mL might be perfect for a heart transplant patient but too high for someone with psoriasis.
One clinic in Sydney started using video tutorials recorded by former patients. One woman, who had a kidney transplant, said: "I didn’t believe the side effects were real until I saw someone else’s story. Then I realized - this could be me if I don’t pay attention."

When to Call Your Doctor - The Red Flags
Not every side effect means disaster. But some do. Patients need to know the difference.
- Call immediately: Fever over 38.5°C, unusual bruising or bleeding, sudden swelling in legs or face, dark urine, or no urine for 12+ hours.
- Call within 24 hours: Tremors, severe headaches, vision changes, or a rash that spreads.
- Don’t wait: If you start a new medication - even something as simple as a cold tablet - check with your doctor first. Many common drugs interact badly with cyclosporine.
There’s no shame in calling. In fact, the best patients are the ones who ask questions before things go wrong.
Tools That Help Patients Stay on Track
Technology can fill the gaps when human support isn’t available.
- Medication apps - Apps like Medisafe or MyTherapy send reminders and track blood test dates. Some even flag drug interactions.
- Smart pill dispensers - Devices like Hero or Pillo dispense pills at set times and alert caregivers if a dose is missed.
- Telehealth check-ins - Many transplant centers now offer biweekly video visits just to review how patients are doing. No blood draw needed - just a quick chat.
One study in 2024 found that patients using a simple smartphone reminder system were 63% less likely to miss a dose than those relying on memory alone.
Family and Caregivers Are Part of the Team
Cyclosporine therapy doesn’t happen in isolation. Spouses, children, or friends often help manage meds, drive to appointments, or notice changes in behavior.
Too often, families are left out of the conversation. But they need to know the same things: what to avoid, what to watch for, and when to call. One mother in Adelaide learned to recognize the early signs of kidney trouble in her teenage son after his transplant - because she was taught what to look for. She called the clinic when he started having headaches and nausea. Tests showed his cyclosporine level had climbed. They adjusted the dose before he needed dialysis.
Include caregivers in every education session. Give them copies of the same handouts. Let them ask questions. Their eyes and ears are often the first warning system.
Education Doesn’t End After the First Month
Patients think once they’ve been on cyclosporine for a while, they "know it all." That’s when the risks spike.
Over time, your body changes. Your kidneys might slow down. Your diet might change. You might start taking a new supplement for joint pain. None of that was true when you started. But your cyclosporine dose might still be the same.
Re-education isn’t optional. Every six months, patients should review their regimen with a pharmacist or nurse. Even if nothing’s changed - because something always changes.
Bottom Line: Knowledge Is the Safest Dose
Cyclosporine saves lives. But it can also take them - if the person taking it doesn’t understand how to use it. The drug doesn’t care if you’re busy, tired, or confused. It reacts to what you give it.
The best outcome isn’t just a functioning transplant or a clear skin rash. It’s a patient who knows exactly what they’re taking, why it matters, and when to speak up. That’s not magic. That’s education.
If you’re on cyclosporine, don’t wait for a crisis to learn. Ask for a detailed review. Bring someone with you. Write down your questions. Keep a log of your doses and symptoms. Your life depends on it - not on the pill, but on what you do with it.
Can I drink alcohol while taking cyclosporine?
Moderate alcohol is usually okay, but it can increase your risk of liver damage and high blood pressure - both already concerns with cyclosporine. Most doctors recommend limiting alcohol to one drink a day or less. Never binge drink. Always check with your transplant team before drinking, especially if your liver function tests are borderline.
How often do I need blood tests for cyclosporine?
When you first start, you’ll need tests every week or two. After a few months, if your levels are stable, it might drop to every 1-3 months. But if you get sick, start a new medicine, or change your diet, your doctor will likely order a test right away. Never skip a blood test just because you feel fine.
Can cyclosporine cause weight gain?
Yes, but not directly. Cyclosporine can cause fluid retention and increased appetite, especially in the first few months. Some patients gain 5-10 kg. This isn’t fat - it’s often water. But it can lead to high blood pressure and strain on the heart. Diet and exercise help, but always talk to your doctor before starting a weight-loss plan - some diets interfere with cyclosporine.
Is cyclosporine safe for long-term use?
It can be, but only with careful monitoring. Long-term use increases the risk of kidney damage, high blood pressure, and certain cancers - especially skin cancer. That’s why patients are advised to use sunscreen daily, avoid sun exposure, and get regular skin checks. Many doctors switch to other immunosuppressants after a few years if possible, to reduce these risks.
What should I do if I miss a dose of cyclosporine?
If you miss a dose and remember within 6 hours, take it right away. If it’s been more than 6 hours, skip the missed dose and take your next one at the regular time. Never double up. Missing doses can trigger organ rejection, so it’s better to skip than to overdose. Always tell your doctor if you miss more than one dose in a month.
Are there natural supplements I should avoid with cyclosporine?
Yes. Many supplements can dangerously raise or lower cyclosporine levels. Avoid St. John’s Wort, echinacea, garlic supplements, and high-dose vitamin E. Even green tea extract and fish oil can interfere. Always tell your doctor about every supplement - even if you think it’s "natural" or "safe."
Next Steps for Patients on Cyclosporine
If you’re taking cyclosporine, here’s what to do today:
- Review your last blood test result. Do you know your trough level?
- Check your pill bottle. Are you taking it at the same time every day, before meals?
- Look at your medicine cabinet. Are there any OTC painkillers, cold meds, or supplements you’re using? Write them down.
- Call your pharmacy or clinic. Ask for a free medication review with a pharmacist.
- Bring a family member to your next appointment. Make sure they know what to watch for.
Small steps. Big impact. Cyclosporine works - but only if you do too.

Hannah Machiorlete
November 19 2025I had a friend on cyclosporine after a kidney transplant. She started taking grapefruit juice because she thought it was 'healthy.' Ended up in the ER with kidney toxicity. No joke. This post is spot on. Don't be that person.