In the realm of gastrointestinal health, the interplay between ulcerative colitis and colon cancer captures significant attention. For those navigating life with ulcerative colitis, the shadow of a possible progression to colon cancer often looms. This connection between chronic inflammation and malignancy is not just a trivial detail—it holds a crucial place in understanding and managing health risks.
The lining of the colon in individuals with ulcerative colitis is persistently inflamed, a condition that can eventually foster an environment conducive to cancerous changes. By delving into how ulcerative colitis can potentially pave the way for colon cancer, one can identify key warning signs early on. Initiating timely screenings and embracing protective dietary and lifestyle habits can significantly alter outcomes.
Understanding Ulcerative Colitis
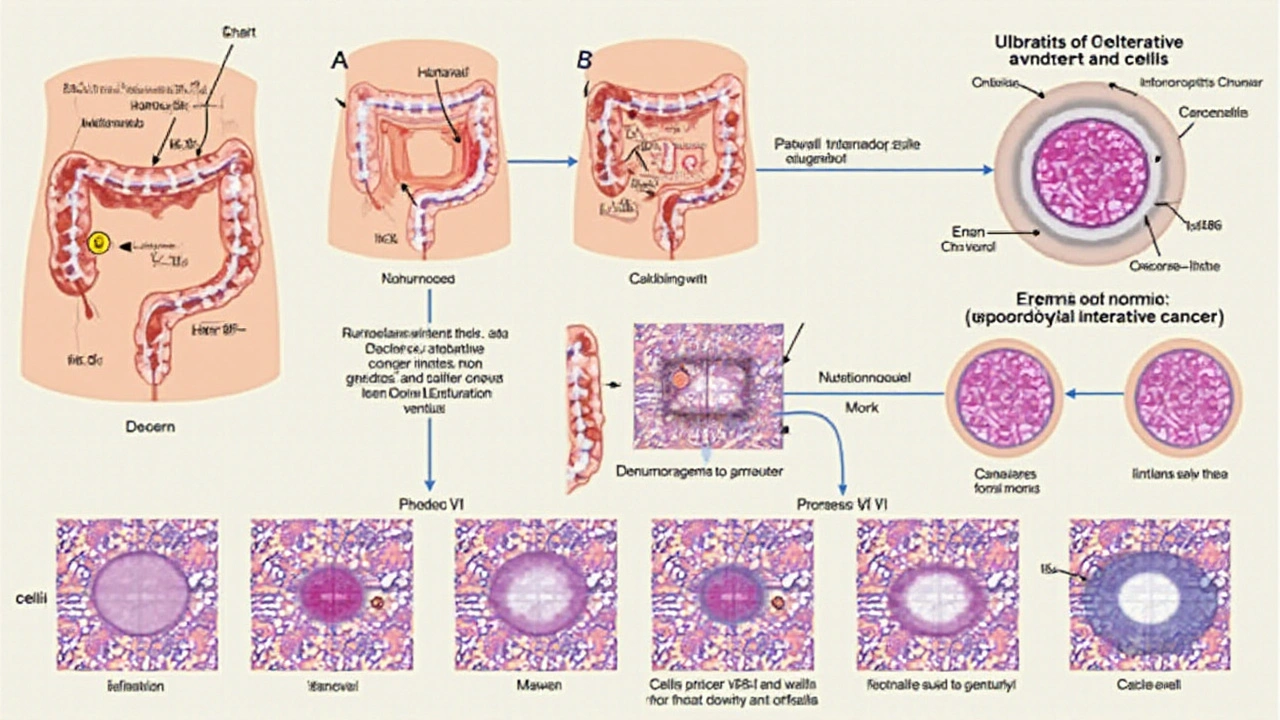
Ulcerative colitis is a chronic inflammatory bowel disease primarily affecting the colon, or large intestine. It manifests through a myriad of symptoms, each varying in intensity from one individual to another. The condition is characterized by continuous stretches of inflammation without the healthy portions seen in its close counterpart, Crohn's disease. This inflammation is not just a fleeting episode; instead, it leads to the prolonged presence of ulcers on the innermost lining of the colon and rectum. People diagnosed with ulcerative colitis often experience periods of relative calm interspersed with intense flares. These flares are marked by a rapid worsening of symptoms, leaving individuals in significant discomfort. Common indications include abdominal pain, frequent diarrhea often mixed with blood, and an urgent need to evacuate the bowels. It is essential to understand that ulcerative colitis's origin lies in the immune system mistakenly attacking the body's own cells, which doctors are still trying to fully comprehend.
The science behind ulcerative colitis involves both genetic and environmental components. Studies have shown a higher prevalence in families with a history of the condition, suggesting a genetic predisposition. Environmental factors might include dietary habits, lifestyle choices, or even levels of urban pollution. Still, despite significant scientific inquiry, no exact cause has been pinpointed. What remains clear is that the body's immune response plays a central role in how this disease unfolds. The continuous immune response causes the damage seen in the intestinal lining, leading to symptoms that can disrupt daily life. Treating and managing ulcerative colitis often requires a comprehensive approach that may involve medication, dietary adjustments, and occasionally surgery.
The emotional and psychological toll of living with ulcerative colitis cannot be understated. The unpredictability of flare-ups introduces significant stress, not only affecting the physical health of patients but also impacting mental well-being. Options like counseling or support groups can be instrumental, offering a safe space to share experiences and coping strategies. Patients are encouraged to openly discuss these aspects with healthcare providers to ensure a holistic approach to treatment.
As Dr. John Smith from the International Gastrointestinal Association aptly says, "Addressing ulcerative colitis requires more than treating just the symptoms; it's about understanding the person as a whole."
Managing ulcerative colitis successfully entails an effective partnership between healthcare providers and patients. Medications like anti-inflammatory drugs, immunosuppressants, or biologics form the cornerstone of treatment plans. These drugs can help to minimize flare-ups and maintain remission. Diet also plays an integral role; some patients find that specific foods can aggravate their symptoms. Identifying and avoiding these foods can make a significant difference in day-to-day comfort and quality of life. For some, surgical intervention becomes necessary when medications no longer provide relief. In these cases, removing the colon might offer a permanent solution, albeit with lifestyle adjustments required post-surgery. Ultimately, early and consistent involvement with specialist care is paramount to finding a suitable management strategy tailored to individual needs.
Link to Colon Cancer
Unraveling the connection between ulcerative colitis and colon cancer reveals insights not just beneficial for medical professionals, but for anyone concerned about their gut health. To understand why individuals with ulcerative colitis possess a markedly higher risk of developing colon cancer, it is essential to grasp the chronic dynamics that unfold within the colon. At the heart of ulcerative colitis lies persistent inflammation, creating an environment that often facilitates the formation of dysplastic cells. These abnormal cells have the potential to transform into cancerous ones over time, significantly increasing colon cancer risk after a prolonged period. The transition from inflammation to cancer isn't typically a rapid process, but one that progresses over several years if unchecked. Regular monitoring and proactive pediatric management are often advised for sustained gut health.
Scientific studies have consistently highlighted this risk. For instance, research has shown that individuals with ulcerative colitis for more than ten years have a considerably elevated chance of developing colon cancer compared to the general population. Interestingly, the risk correlates closely with both the duration and extent of the disease—patients experiencing pancolitis or inflammation affecting the entire colon face the highest risks. Dr. John Smith, an expert in colon research, aptly noted,
"The relentless inflammation observed in ulcerative colitis is akin to a slow-burning fire, one that quietly sets the stage for malignancy in susceptible individuals."These findings underscore the importance of vigilance and regular medical assessments.
Thus, for those living with ulcerative colitis, it's vital to consider guidelines for cancer prevention. Colonoscopies, for example, play a significant role in surveillance, allowing for early detection of precancerous changes. Early intervention and treatment can greatly influence outcomes. Other preventive strategies include adhering to dietary recommendations that promote gut health. Foods rich in antioxidants and beneficial fibers are often highlighted, encouraging a diversified microbiome and reducing inflammation. Moreover, lifestyle choices such as smoking cessation, maintaining a healthy weight, and regular exercise might also lower the risk of colon cancer.
The relationship between ulcerative colitis and colon cancer stands as a testament to the intricate workings of the human body. Despite the challenges posed by chronic inflammation, understanding the nuances of this link opens doors to proactive care strategies. Individuals are not just passive spectators in this journey but active participants in mitigating cancer risks associated with their condition. Embracing a lifestyle conducive to well-being, staying informed, and collaborating with healthcare practitioners form the pillars of an empowered approach to managing ulcerative colitis and its potential implications.

Symptoms to Monitor
When it comes to understanding the symptoms that might indicate a shift from ulcerative colitis towards more serious conditions like colon cancer, vigilance is key. Although many symptoms of these diseases can overlap, there are certain nuances that might help distinguish a simple flare-up from something more concerning. For those living with ulcerative colitis, it's important to be acutely aware of changes in their usual pattern of symptoms, as any significant alteration might warrant further investigation.
Typically, individuals with ulcerative colitis experience abdominal pain and cramping, but an escalation in severity or frequency could be cause for concern. An unanticipated change in bowel habits, such as constant diarrhea that doesn't respond to usual treatments, should not be dismissed lightly. Blood in the stool is another symptom that, while common in ulcerative colitis, can point to colon cancer if it worsens without any apparent reason or is accompanied by significant weight loss and fatigue. In terms of gut health, persistent symptoms like these might indicate that it's time to consult a healthcare professional for more comprehensive testing.
Pay Attention to Unusual Changes
Another aspect to consider is the onset of anemia, which can manifest as unexplained tiredness or paleness, and should always be followed up with a doctor's visit. Similarly, a new occurrence of intense abdominal discomfort or a noticeable mass in the abdomen could raise red flags. It's worth noting that these symptoms might appear gradually, which stresses the importance of regular monitoring and medical oversight. In a testimonial by Dr. Arnold Silverberg, a renowned gastroenterologist, he emphasizes,
"Any new or worsening symptoms in colitis patients should be thoroughly evaluated promptly to rule out malignancy."His advice highlights the delicate balance of being aware but not alarmed, understanding that early detection is crucial.
Consult with Medical Professionals
With disease prevention being a goal for those with ulcerative colitis, regular screenings and check-ups with healthcare providers can make a significant difference. By keeping track of medical history and symptoms through detailed records, patients can aid their doctors in spotting patterns that might indicate deeper issues. Considering the sometimes subtle nature of symptom evolution, open communication with healthcare providers becomes essential in ensuring the correct measures are taken in a timely manner. Finally, embracing a proactive health approach can not only improve quality of life but also reduce anxiety related to potential complications.

Preventive Measures
When grappling with chronic conditions such as ulcerative colitis, taking proactive steps becomes imperative in mitigating the heightened risk of developing colon cancer. A cornerstone of preventive strategies is regular screenings, as early detection can make a world of difference. People diagnosed with ulcerative colitis are often advised to start colon cancer screenings earlier and more frequently than the general population. The colonoscopy remains a crucial tool, not merely for detection, but also in preventing cancer by allowing the removal of any abnormal precancerous lesions that may be discovered during the procedure.
Dietary choices also play a pivotal role in nurturing gut health. Consuming a diet rich in fruits, vegetables, whole grains, and lean proteins can provide the nutrients necessary to maintain a healthy colon environment. These foods are abundant in fiber, which promotes regular bowel movements and may assist in reducing inflammation. Moreover, reducing intake of red meat and processed foods, which have been linked to increased cancer risk, can be beneficial. Maintaining a balanced diet is more than just filling your plate—it's about creating an anti-inflammatory environment within the body.
Incorporating Lifestyle Modifications
In addition to dietary management, incorporating regular physical activity into one's routine can offer substantial benefits. Exercise helps stimulate digestion and reduce inflammation, and it's known to boost overall immune function. Even moderate daily exercise, like walking or cycling, promotes a healthier lifestyle, reducing the risks associated with both ulcerative colitis and colon cancer. Stress management techniques, including yoga, meditation, and deep-breathing exercises, can also be important. Chronic stress has been linked to increased inflammation, so employing methods to manage stress can be crucial for those with ulcerative colitis.
Medical therapy is another vital component. If you are dealing with ulcerative colitis, adhering to prescribed medications can help control inflammation and avert complications. Citrulline-based medications, aminosalicylates, corticosteroids, and immunomodulators might be part of a treatment regimen that minimizes risks. Recent advancements have seen the introduction of biologic agents that target specific pathways associated with inflammation, offering hope for more targeted therapeutics. However, these treatments should be approached with careful consideration and regular dialogue with healthcare providers.
Evidence continues to evolve on the role of supplements. Incorporating omega-3 fatty acids, widely found in fish oil, may play a role in reducing inflammation. Likewise, probiotics, found in certain yogurts and available as supplements, foster beneficial gut bacteria and may help maintain intestinal health. While supplements shouldn't replace a balanced and nutritious diet, they can offer additional support, especially in consultation with healthcare professionals.
"Regular check-ups and consulting with your healthcare provider about any change in symptoms is crucial," advises Dr. Clara Lindholm, a gastroenterologist at the renowned Gut Health Institute. "Prevention is a combination of lifestyle choices, medical compliance, and vigilant monitoring."
By taking steps to monitor and adapt healthy lifestyle choices, those living with ulcerative colitis can significantly diminish the risk of colon cancer. It doesn't come down to a single factor, but rather an integrated approach encompassing medical advice, dietary modifications, and lifestyle adjustments to safeguard against these complications.


Leah Hawthorne
January 23 2025Living with ulcerative colitis feels like walking a tightrope where every step could trigger a flare. The chronic inflammation isn’t just a symptom; it’s a constant reminder that the gut lining is under assault. Over time, that relentless irritation can set the stage for dysplasia, which is the stepping stone toward malignancy. It’s why gastroenterologists stress the importance of early and regular colonoscopic surveillance. I’ve seen patients who ignored the recommended screening schedules and later faced a tougher battle with cancer. On the flip side, those who stick to a strict monitoring routine often catch precancerous changes when they’re still manageable. Diet plays a surprisingly big role too-high-fiber foods, leafy greens, and omega‑3s can help dampen inflammation. Equally important is staying active; even light exercise improves gut motility and reduces stress hormones that can flare the disease. Stress management isn’t just a buzzword; chronic stress can elevate cortisol and aggravate the immune response. Some people find meditation or yoga effective, while others rely on journaling to track symptom patterns. Medication adherence can’t be overstated-missing a dose of aminosalicylates or biologics can let inflammation creep back in. For those considering surgery, a total proctocolectomy eliminates cancer risk but comes with lifestyle adjustments that need careful planning. It’s a trade‑off that has to be weighed with a specialist. I also recommend regular blood work to monitor anemia, which can be an early sign of hidden bleeding. Lastly, community support groups provide an outlet for sharing tips and emotional support, which can be a lifesaver during tough flare‑ups.