Blood Thinner Time Zone Calculator
Enter your current time and destination time zone to calculate the correct medication time. This tool accounts for differences between DOACs and Warfarin dosing requirements.
Traveling while on blood thinners doesn’t have to be scary-but it does require planning. Whether you’re flying to Europe, hiking in Southeast Asia, or cruising the Caribbean, your medication schedule, diet, and movement habits all matter more than ever. The goal isn’t to avoid travel-it’s to manage your treatment so you stay protected from clots without putting yourself at risk for dangerous bleeding.
Know Your Medication: DOACs vs. Warfarin
If you’re on a blood thinner, the first thing you need to know is which kind you’re taking. There are two main types: warfarin and DOACs (direct oral anticoagulants). They work differently, and that changes how you travel.Warfarin has been around for decades. It’s cheap and effective, but it demands constant attention. You need regular blood tests to check your INR (International Normalized Ratio), which tells doctors if your blood is thinning enough. Most people aim for an INR between 2.0 and 3.0. If it’s too low, you risk clots. Too high, and you could bleed internally. That’s why warfarin users carry a yellow booklet with their test results and dosing history. You need it when you’re abroad-medical staff won’t know your history unless you show it.
DOACs like apixaban, rivaroxaban, dabigatran, and edoxaban are newer. They don’t need blood tests. Their dosing is predictable, and they have fewer interactions with food and other drugs. For travelers, this is a game-changer. You don’t have to hunt for a lab in Bali or negotiate with a clinic in Mexico to check your levels. You just take your pill, stick to the schedule, and you’re covered.
But here’s the catch: DOACs leave your system faster. They work for 12 to 24 hours, so skipping a dose-even once-can leave you unprotected. Warfarin lingers longer, so missing a day isn’t as urgent. But that doesn’t mean you can be careless. Both types require discipline.
Time Zones Are Your Enemy (And How to Beat Them)
Changing time zones messes with your routine. You might wake up late, eat at odd hours, or forget your pill because you’re jet-lagged. That’s dangerous.For DOAC users: Try to take your dose at the same time each day, even if the clock changes. If you’re flying from Melbourne to New York and lose 16 hours, don’t take your pill at 8 a.m. Melbourne time and then again at 8 a.m. New York time. That could mean two doses in one day. Instead, adjust gradually. If you normally take your pill at 8 p.m., keep taking it at 8 p.m. local time. Use phone alarms. Set two: one for your original time zone, one for your destination. That way, you won’t accidentally double-dose or skip.
Warfarin users have a tougher job. Your INR is affected by what you eat-especially vitamin K, found in leafy greens like spinach, kale, and broccoli. A salad in Paris might be fine. A big bowl of collard greens in Georgia? That could spike your INR and make you bleed. Stick to familiar foods. Avoid new superfoods or exotic greens unless you’re sure about their vitamin K content. And if you’re going to be eating differently for more than a week, talk to your doctor about adjusting your dose before you leave.
Hydration, Alcohol, and What You Drink
Dehydration thickens your blood. That’s the last thing you want when you’re on a blood thinner. Airplanes are dry. Long car rides? Same thing. Alcohol? Even worse. It dehydrates you and can interfere with how your liver processes your medication.Stick to water. Drink at least 8 ounces every hour on long flights. Skip the cocktails, soda, and even too much coffee. If you’re going out for dinner, have one glass of wine at most. And never mix alcohol with your pill. It increases bleeding risk without helping your clot protection.
Move or Risk a Clot
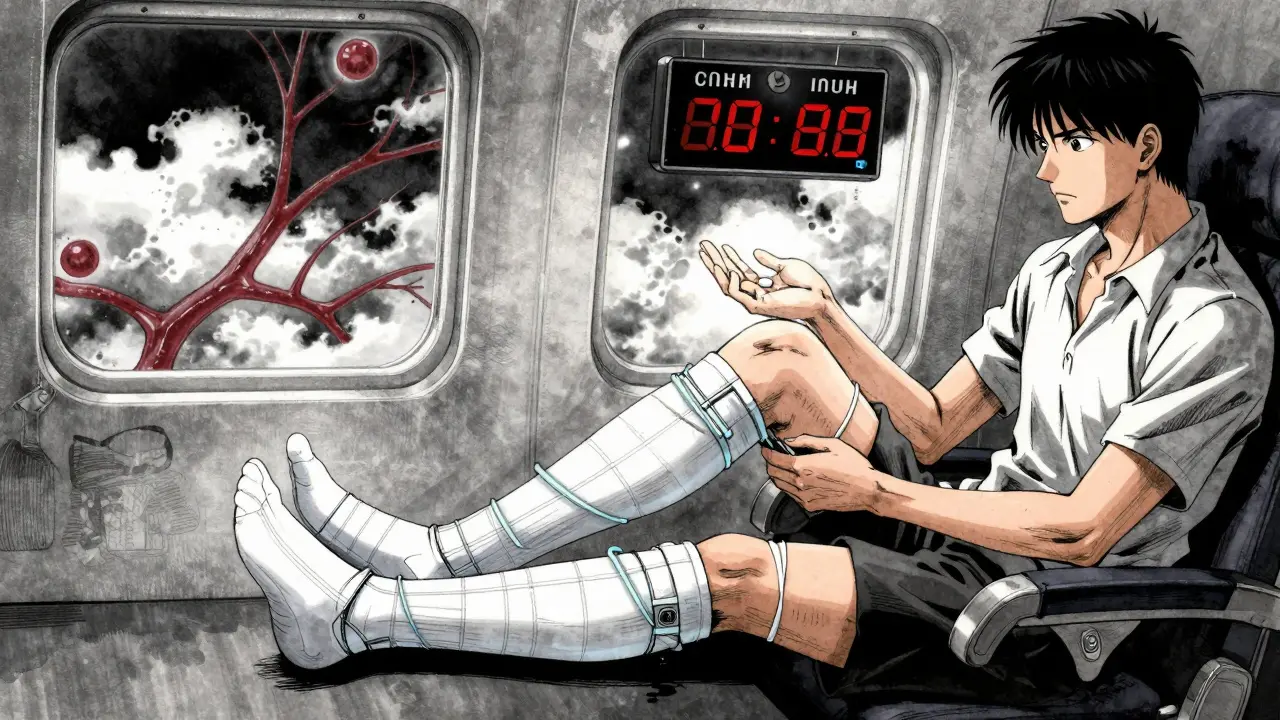
Sitting still for hours-especially on flights longer than six hours-is one of the biggest triggers for deep vein thrombosis (DVT). That’s when a clot forms in your leg. If it breaks loose, it can travel to your lungs and cause a pulmonary embolism (PE), which can be deadly.Don’t wait until your leg feels stiff. Get up and walk every two to three hours. If you’re in a window seat and can’t get up easily, do seated exercises. Point your toes up toward your shins. Circle your ankles. Squeeze your calf muscles. Do this every 30 minutes. It’s not optional. It’s as important as taking your pill.
Wear compression socks. They’re not just for pregnant women or older travelers. If you’re on blood thinners, they add an extra layer of protection. Choose medical-grade, graduated compression-20 to 30 mmHg. Don’t buy the cheap ones at the airport. They won’t help.
What to Pack (And What to Leave Behind)
Your pill bottle isn’t enough. You need a travel kit.- For DOAC users: Bring at least 1.5 times your supply. Flights get delayed. Borders close. Pharmacies abroad might not carry your brand. Keep your pills in their original bottles with the prescription label. Carry a copy of your prescription too.
- For warfarin users: Bring your yellow booklet. Bring extra tablets in different strengths (1mg, 2mg, 5mg). You might need to adjust your dose if you’re sick or eating differently. Don’t rely on foreign pharmacies to have the same brand or dosage.
- Always carry a medical ID card or bracelet that says you’re on anticoagulants. Include your medication name, dose, and emergency contact.
- Bring a small first-aid kit with gauze, tape, and a clotting agent like QuikClot. If you cut yourself, you’ll bleed longer. Be ready.
Never pack your pills in checked luggage. If your bag gets lost, you’re stuck. Keep them in your carry-on, with your passport and wallet.
Avoid High-Risk Activities
Some activities are just too risky. Diving? Not recommended if you’re on warfarin. Changes in pressure can cause bleeding in your ears, spine, or brain. Even if you’ve done it before, the risk isn’t worth it. Skiing? Be careful. Falls are common. If you’re on a DOAC, you might be okay with moderate skiing-but wear a helmet and avoid black diamonds.Adventure sports like rock climbing, skydiving, or contact sports? Skip them. Your body doesn’t heal the same way when you’re thinning your blood. A minor bump could turn into a serious bleed.

What to Do If You Feel Something’s Wrong
You might feel fine-until you don’t. Signs of a clot include swelling, warmth, or pain in one leg. Red streaks. Sudden shortness of breath. Chest pain. A headache that won’t quit. A nosebleed that won’t stop. Unexplained bruising. These aren’t normal.If you notice any of these, get help immediately. Don’t wait. Don’t think it’s just jet lag. Emergency rooms worldwide are used to treating people on blood thinners. They know how to test for clots and manage bleeding. But you have to speak up. Tell them you’re on anticoagulants. Show them your booklet or prescription. Say it clearly: “I’m on blood thinners.”
Early help means you’ll likely avoid hospitalization. Delayed care? That’s when trips turn into emergencies.
When Not to Travel
If you’ve had a recent clot-within the last four weeks-don’t travel. Not even for a weekend. Your body is still healing. The risk of another clot is highest right after treatment starts. Your doctor will tell you when it’s safe. Wait. It’s not worth the gamble.Also, if you’re planning to go somewhere with poor medical access-remote areas, developing countries without reliable labs or emergency care-talk to your doctor first. DOACs are safer here, but you still need access to care if something goes wrong.
Bottom Line: Plan, Pack, Move
Traveling with blood thinners isn’t about fear. It’s about smart habits. Know your meds. Stick to your schedule. Drink water. Move often. Pack extra. Carry your docs. Avoid risky activities. And never assume you’ll be fine just because you’ve done it before.The best travelers on blood thinners aren’t the ones who never get sick. They’re the ones who planned ahead-and didn’t take chances.
Can I fly if I’m on blood thinners?
Yes, you can fly. But you need to take precautions. Stay hydrated, move every two hours, wear compression socks, and never skip your dose. DOACs are easier to manage on flights because they don’t require blood tests. Warfarin users should carry their INR booklet and avoid major dietary changes before flying.
What happens if I miss a dose of my blood thinner?
If you miss one dose of a DOAC, take it as soon as you remember-if it’s within 12 hours of your usual time. If it’s more than 12 hours late, skip it and take your next dose at the regular time. Never double up. For warfarin, missing one day isn’t as urgent, but don’t make it a habit. If you miss more than one day, contact your doctor. Your INR could drop, raising your clot risk.
Are DOACs safer than warfarin for travel?
Yes, for most travelers. DOACs don’t need blood tests, have fewer food interactions, and work predictably. Warfarin requires strict diet control and regular INR monitoring, which is hard to manage abroad. DOACs are now the standard for most patients, including those traveling. But both are safe if used correctly.
Can I drink alcohol while on blood thinners?
Limit it. One drink occasionally is usually okay, but alcohol dehydrates you and can increase bleeding risk. It also interferes with how your liver breaks down warfarin. Avoid binge drinking. Never mix alcohol with your pill. Stick to water, especially on flights and in hot climates.
What should I do if I get sick while traveling?
Don’t take over-the-counter meds without checking. Some painkillers like ibuprofen and aspirin can increase bleeding risk. Use acetaminophen (paracetamol) instead for fever or pain. Stay hydrated. Rest. If you have vomiting, diarrhea, or a fever for more than 24 hours, contact a local doctor. Illness can change how your body processes blood thinners, especially warfarin.
If you’ve been cleared to travel, don’t let fear hold you back. Millions of people on blood thinners fly, hike, and explore every year. The key isn’t avoiding travel-it’s preparing for it like a pro.


Katie Taylor
December 23 2025Okay but let’s be real-DOACs are the MVP of travel meds. I flew to Thailand last year on rivaroxaban, didn’t even think about it. Just set phone alarms, drank water like it was my job, and did ankle circles on the plane like a maniac. No drama. No labs. No panic. Warfarin folks? You’re the real heroes. I couldn’t do that.