Skin inflammation makes your skin red, sore, itchy, or swollen. It can show up as a small patch of rash or a bigger area that gets hot and painful. You don’t always need a doctor, but knowing what’s likely causing it and how to act fast helps you feel better and avoid problems.
There are lots of reasons skin gets inflamed. Allergic contact (like nickel or certain perfumes), irritants (harsh soaps, detergents), insect bites, infections (bacterial or fungal), and chronic conditions such as eczema or psoriasis are top culprits. Typical signs include redness, itching, warmth, swelling, and sometimes blisters or peeling. If the area has pus, spreading redness, fever, or severe pain, that often points to an infection and needs medical attention.
Think about timing and triggers. A new soap, a plant you touched, or a medication change can clue you in. For chronic flare-ups, note diet, stress, and weather—dry cold air or sweating can worsen inflammation. Keep a small log on your phone: date, what you used on the skin, foods you ate, and any symptoms. That helps your doctor or pharmacist spot patterns faster.
Start simple: cool compresses and gentle washing with lukewarm water help most minor flares. Avoid scrubbing. Switch to a fragrance-free, mild cleanser and apply a plain moisturizer while the skin heals. Over-the-counter topical hydrocortisone can reduce redness and itching for short periods. For fungal rashes, antifungal creams work well; for bacterial infections, you might need antibiotics—topical or oral—so check with a provider if it looks infected.
If you have eczema, regular moisturizing and avoiding known triggers are the main game. Prescription options include stronger topical steroids and non-steroidal creams; for stubborn cases, doctors may suggest oral treatments or light therapy. When inflammation follows an insect bite or minor allergic reaction, antihistamines can cut the itch and help you sleep.
When to see a doctor: signs that mean go now include spreading redness, fever, severe pain, pus, or if the rash affects your face or genitals. Also get help if home care doesn’t improve things in a few days, or if flare-ups keep coming back. A clinician can test for infection, prescribe the right antibiotic or steroid, and rule out serious causes.
Practical tips to prevent repeats: choose gentle skin products, wear breathable fabrics, patch-test new cosmetics, and keep nails short to avoid breaking the skin when you scratch. If you suspect a product or food allergy, consider talking to an allergist for testing. Small habit changes often cut flare-ups dramatically.
Skin inflammation is common and usually manageable with smart home care and medical help when needed. Track patterns, act early, and ask for help if it gets worse—your skin usually recovers faster that way.
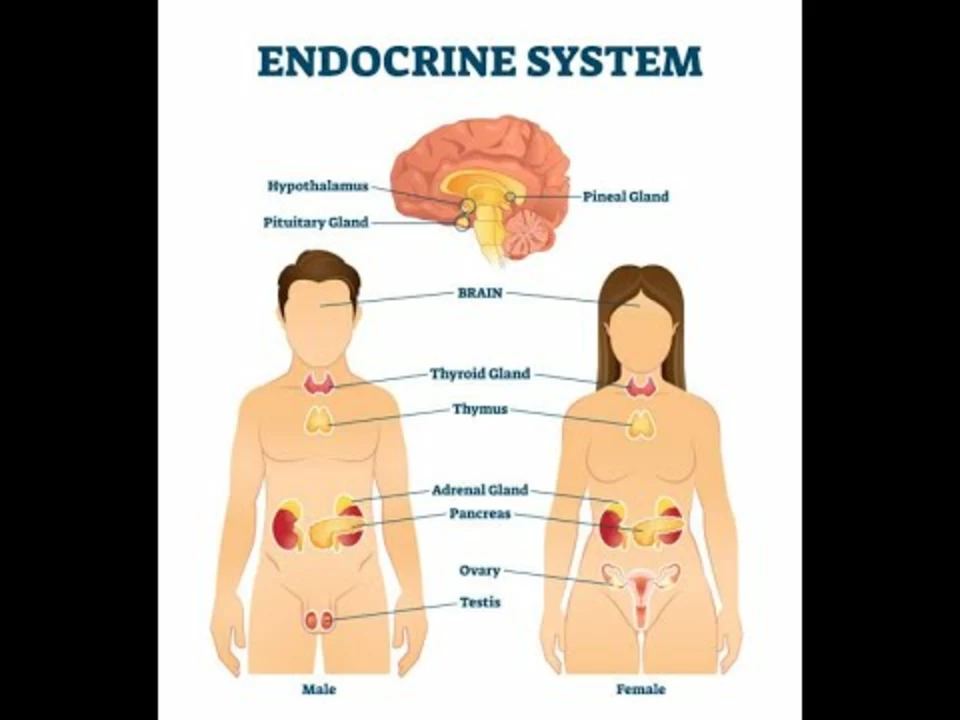
In a recent exploration of the link between hormonal imbalances and atopic dermatitis, I discovered that our hormones can play a significant role in the development and severity of this skin condition. Fluctuations in hormones, such as during pregnancy or puberty, can exacerbate atopic dermatitis symptoms. Stress, which affects our cortisol levels, can also contribute to worsening skin issues. Furthermore, individuals with thyroid disorders may experience more severe atopic dermatitis due to imbalances in their hormone production. Overall, understanding and addressing these hormonal imbalances could lead to more effective treatments and management strategies for atopic dermatitis sufferers.