When quadruple therapy, a four-drug regimen used to eradicate Helicobacter pylori infections is prescribed, it’s usually because simpler treatments didn’t work. This isn’t a first-line option—it’s the backup plan doctors turn to when standard triple therapy fails, or when resistance to common antibiotics like clarithromycin is high. It combines a proton pump inhibitor, a medication that reduces stomach acid to help healing and improve antibiotic effectiveness, two antibiotics, drugs chosen to kill H. pylori bacteria while minimizing resistance, and sometimes bismuth subsalicylate, a protective agent that also has antibacterial properties. Together, these four components attack the infection from multiple angles, making it harder for the bacteria to survive.
Quadruple therapy is most commonly used for H. pylori, the bacteria responsible for most peptic ulcers and chronic gastritis. It’s especially important in areas where clarithromycin resistance is above 15%, which includes much of the U.S. and Europe. The typical combo includes a proton pump inhibitor like omeprazole or esomeprazole, plus two antibiotics—often metronidazole and tetracycline, or amoxicillin and metronidazole—and bismuth subsalicylate (like Pepto-Bismol). Treatment lasts 10 to 14 days, and success rates can hit 90% when taken exactly as directed. Missing doses or stopping early is one of the main reasons it fails. Side effects are common—metallic taste, nausea, dark stools, and diarrhea—but they’re usually manageable and go away after treatment ends.
Doctors don’t pick this regimen lightly. It’s more complex than triple therapy, with more pills and stricter timing. But when your infection won’t budge, it’s often the only thing left that works. Recent studies show it outperforms triple therapy in regions with high antibiotic resistance, and guidelines from the American College of Gastroenterology now recommend it as a preferred option in many cases. It’s also used for patients who’ve had prior exposure to macrolide antibiotics, since those can make standard treatments useless. The key is adherence—taking every pill at the right time, even if you feel fine. This isn’t a quick fix; it’s a full assault on a stubborn bug.
Below, you’ll find real-world insights from patients and providers on how quadruple therapy fits into broader treatment strategies, what to expect during the course, and how it compares to other options for stomach infections and ulcers. These posts don’t just explain the drugs—they show you how the system works behind the scenes, from pharmacy alerts to patient compliance, and why this treatment matters more than you might think.
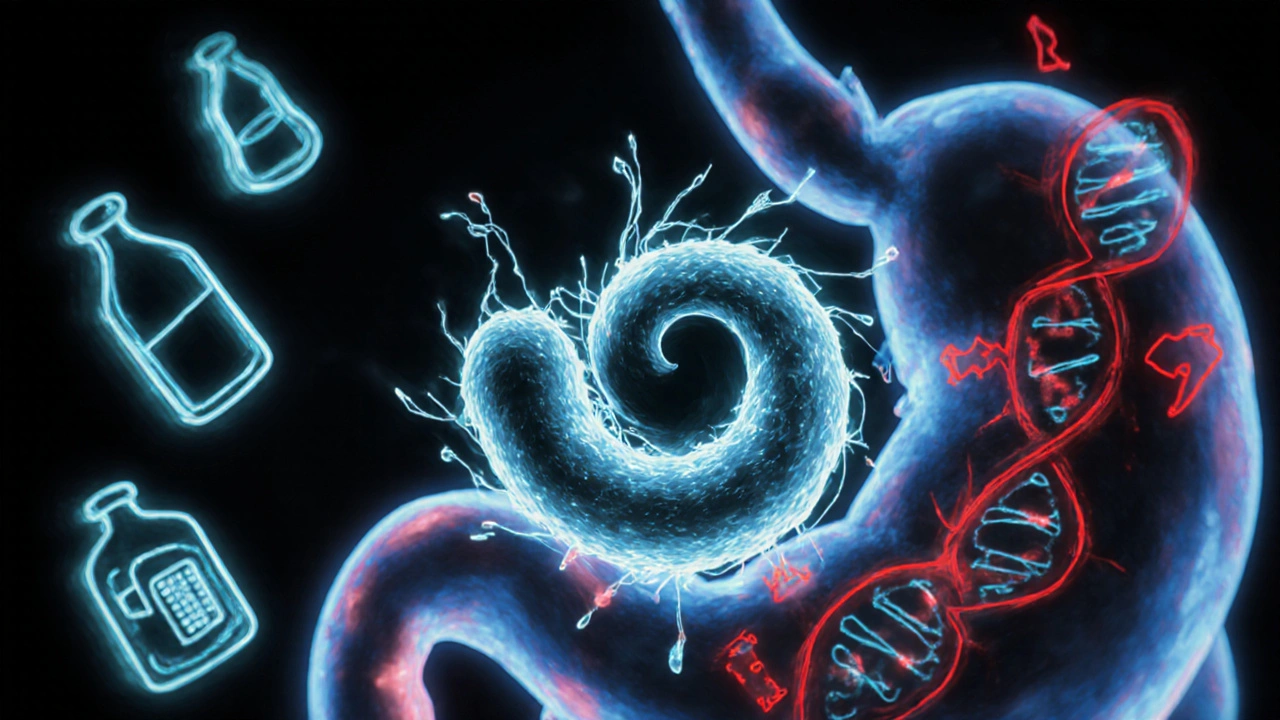
H. pylori infection is common but often undiagnosed. Learn how modern testing and quadruple therapy are replacing outdated treatments to fight rising antibiotic resistance and prevent serious stomach conditions.