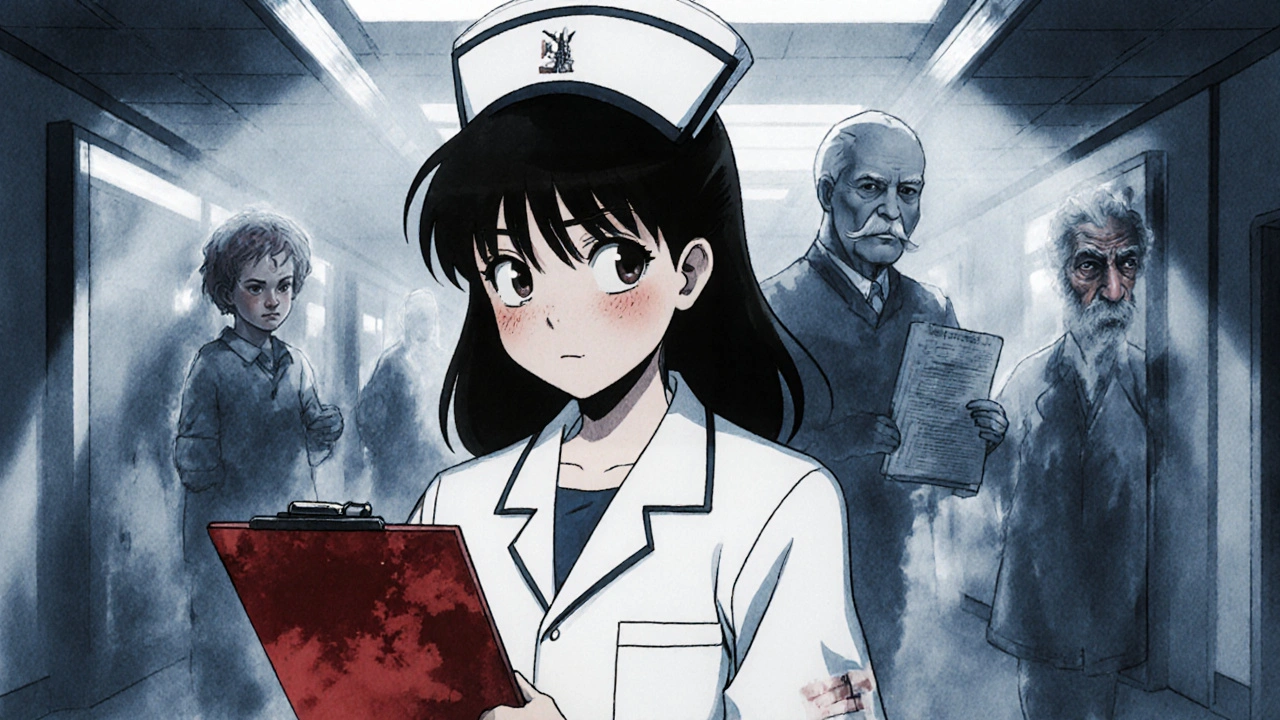
When you take a pill, you trust it’s the right one, at the right dose, for your body. But patient safety, the practice of preventing harm during medical care is often broken before you even leave the pharmacy. It’s not about bad people—it’s about systems that don’t talk to each other, confusing labels, and alerts that mean nothing. You’re not imagining it: mistakes happen more than you think, and you have more power to stop them than you realize.
One of the biggest risks is dose verification, the process of double-checking medication amounts before giving them. A simple typo—0.5 mg instead of 5 mg—can be deadly. That’s why hospitals use double-check protocols, but at home? You’re on your own. And then there’s drug interactions, when two or more medicines react dangerously together. Simvastatin with certain antibiotics? Risk of muscle damage. Cyclosporine mixed with grapefruit juice? Toxic levels. These aren’t rare edge cases—they’re daily threats hidden in your pill bottle. Even pharmacy alerts, the red warnings your pharmacist sees when filling a prescription are often wrong. Studies show up to 90% are false alarms, but if you ignore them all, you might miss the one that saves your life.
It’s not just about what’s in the bottle. It’s about how you talk to your doctor, how you read the label, and whether you know your own allergies. One person took Claritin-D thinking it was just an allergy pill—until their blood pressure spiked. Another skipped their statin because they thought dry mouth meant it wasn’t working. Both were wrong. Patient safety isn’t something hospitals do for you. It’s something you do with them. You’re the only one who knows your body, your history, and your real concerns. If your pharmacist says an alert is a mistake, ask why. If your doctor changes your dose, write it down. If a new pill looks different, ask if it’s the same. These aren’t extra steps—they’re your last line of defense.
Below, you’ll find real stories and clear guides on how to catch errors before they happen—from checking your prescription against the bottle, to understanding why your meds might be interacting, to knowing when to push back when something doesn’t feel right. This isn’t theory. It’s what works when it matters most.
Doctors and nurses must legally report suspected child abuse, elder abuse, public health threats, and professional misconduct. Learn what you need to report, when, and how to do it right to protect patients and avoid legal risk.