When a nurse speaks up about a wrong dose, a missed vital sign, or a confusing order, they’re doing nurse reporting, the process of documenting and communicating critical patient information to ensure safe, continuous care. It’s not just paperwork—it’s the last line of defense against preventable harm. In fact, studies show that over 70% of medication errors are caught by nurses before they reach the patient. That’s not luck. That’s reporting.
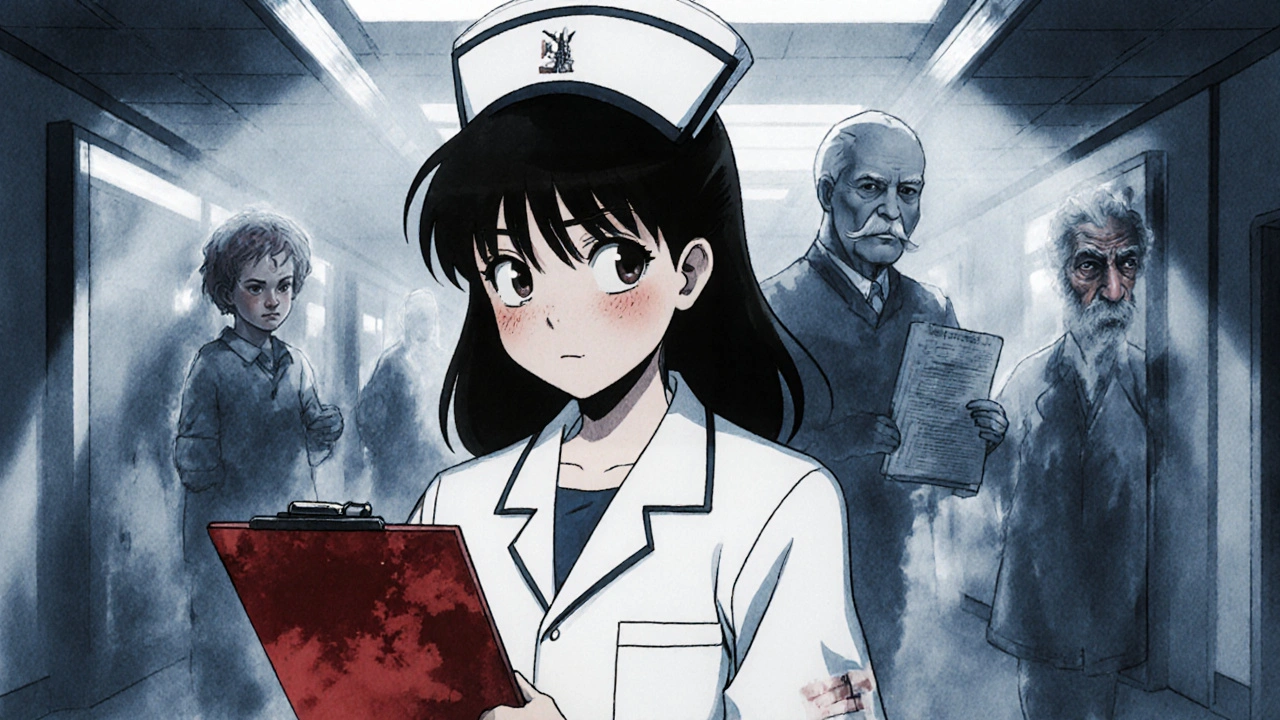
Patient safety, the practice of preventing avoidable harm during medical care depends entirely on how well nurses can share what they see. A nurse might notice a patient’s blood pressure dropping after a new drug is given. If that detail gets lost in a rushed handoff or buried in a messy chart, the consequences can be deadly. Good healthcare communication, the clear, timely exchange of clinical information between providers turns observations into action. And when that system fails—because of fatigue, poor tools, or silence—it’s the patients who pay the price.
Most nurse reporting isn’t dramatic. It’s the quiet moments: checking a label twice, confirming a dose with a pharmacist, writing down a change in breathing pattern, or flagging a family’s concern that no one else noticed. These actions build up. They connect. And they’re the reason why medication errors, mistakes in prescribing, dispensing, or giving drugs that can harm patients drop by nearly half in units with strong reporting cultures. It’s not about blaming someone. It’s about making sure the system hears what the nurse knows.
And then there’s clinical documentation, the official record of patient care that guides treatment and legal protection. It’s not just filling out forms. It’s telling the story of a patient’s day—what changed, what stayed the same, what worried you. If a doctor doesn’t see that a patient’s pain spiked after midnight, they might think the new painkiller isn’t working. But if the nurse documented it clearly, they might realize the dose timing is off. That’s the power of good notes.
You’ll find real examples of this in the posts below. From how to verify dose changes to understanding pharmacy alerts, from managing drug interactions to preventing miscommunication in high-stress environments—every article ties back to one truth: nurses are the eyes and ears of the healthcare system. When they report well, people live longer, recover faster, and feel safer. When they’re ignored, or silenced, or drowned in paperwork, the cost is measured in lives.
What follows isn’t just a list of articles. It’s a collection of tools, stories, and warnings—each one shaped by the real challenges nurses face every shift. Whether you’re a nurse, a student, or someone who’s been on the other side of the bed, these posts will show you how reporting isn’t just part of the job. It’s the heartbeat of safe care.
Doctors and nurses must legally report suspected child abuse, elder abuse, public health threats, and professional misconduct. Learn what you need to report, when, and how to do it right to protect patients and avoid legal risk.