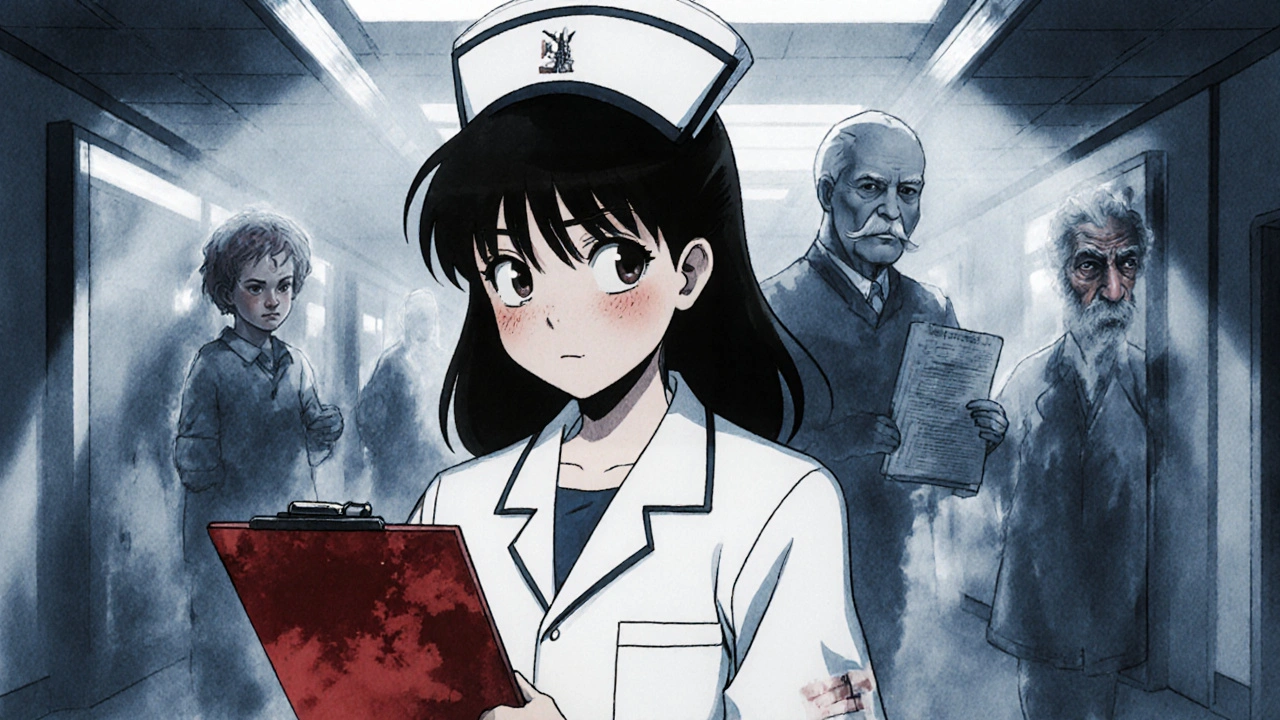
When you hear healthcare reporting, the process of documenting and disclosing medical errors, safety risks, or illegal practices within healthcare systems. Also known as patient safety reporting, it’s not just paperwork—it’s the line of defense between a routine mistake and a life-changing injury. Every time a nurse catches a wrong dose before it’s given, every time a pharmacist flags a dangerous drug combo, and every time a worker speaks up about unsafe conditions, that’s healthcare reporting in action. It’s not about blaming people. It’s about fixing systems before someone gets hurt.
This isn’t just about hospitals. whistleblower laws, legal protections for employees who report illegal or unsafe practices in healthcare settings. Also known as medical whistleblower protections, they give people the courage to come forward without fear of losing their job. In 2025, California strengthened these rules to cover more types of reporting—from hiding infection rates to falsifying medication logs. And it’s not just about fraud. medication errors, mistakes in prescribing, dispensing, or administering drugs that lead to harm. Also known as drug safety incidents, they’re one of the top causes of preventable hospital deaths. A single misread prescription, a missed allergy alert, or a confusing dose change can turn a routine visit into a crisis. That’s why reporting these moments—not to punish, but to learn—is critical.
Behind every report is data. healthcare data, information collected from patient records, pharmacy systems, and clinical workflows used to track safety trends and improve care. Also known as clinical data reporting, it’s what turns one bad event into a system-wide fix. When 10 different pharmacies report the same interaction between a statin and a common antibiotic, regulators don’t just notice—they update guidelines. When a hospital sees a spike in wrong-dose incidents after a new electronic system goes live, they don’t ignore it—they retrain staff. That’s how reporting saves lives: by turning isolated incidents into patterns, and patterns into change.
What you’ll find in this collection aren’t abstract theories. These are real stories from inside pharmacies, clinics, and hospitals—where someone spoke up, checked a dose, questioned a label, or filed a report. You’ll read about how generic substitution affects patient costs, why pharmacy allergy alerts are often wrong, how antibiotic resistance is tracked, and how whistleblowers in California are protected. These aren’t just articles. They’re snapshots of healthcare reporting in the wild—where the stakes are high, the details matter, and the right question can stop a disaster before it starts.
Doctors and nurses must legally report suspected child abuse, elder abuse, public health threats, and professional misconduct. Learn what you need to report, when, and how to do it right to protect patients and avoid legal risk.