When your doctor or pharmacist checks your EHR allergy system, a digital tool that stores and alerts healthcare providers about your known drug allergies. Also known as electronic allergy documentation, it’s meant to stop a life-threatening reaction before it starts. But too often, it’s just a checkbox on a screen—missing critical details, outdated, or ignored. That’s not how it’s supposed to work.
A real EHR allergy system doesn’t just say "penicillin allergy." It tells you what kind of reaction you had—rash, swelling, anaphylaxis—and when it happened. It links to your current meds, flags risky combinations, and warns pharmacists before they dispense a substitute. It’s not magic. It’s data. And if your system only records "allergy: yes," you’re playing Russian roulette with your health. The electronic health records, digital versions of your medical history used by clinics and hospitals. Also known as EMR, they’re the backbone of modern care should be smarter than that. Studies show that poorly documented allergies lead to 1 in 5 avoidable adverse drug events. That’s not a glitch—it’s a system failure.
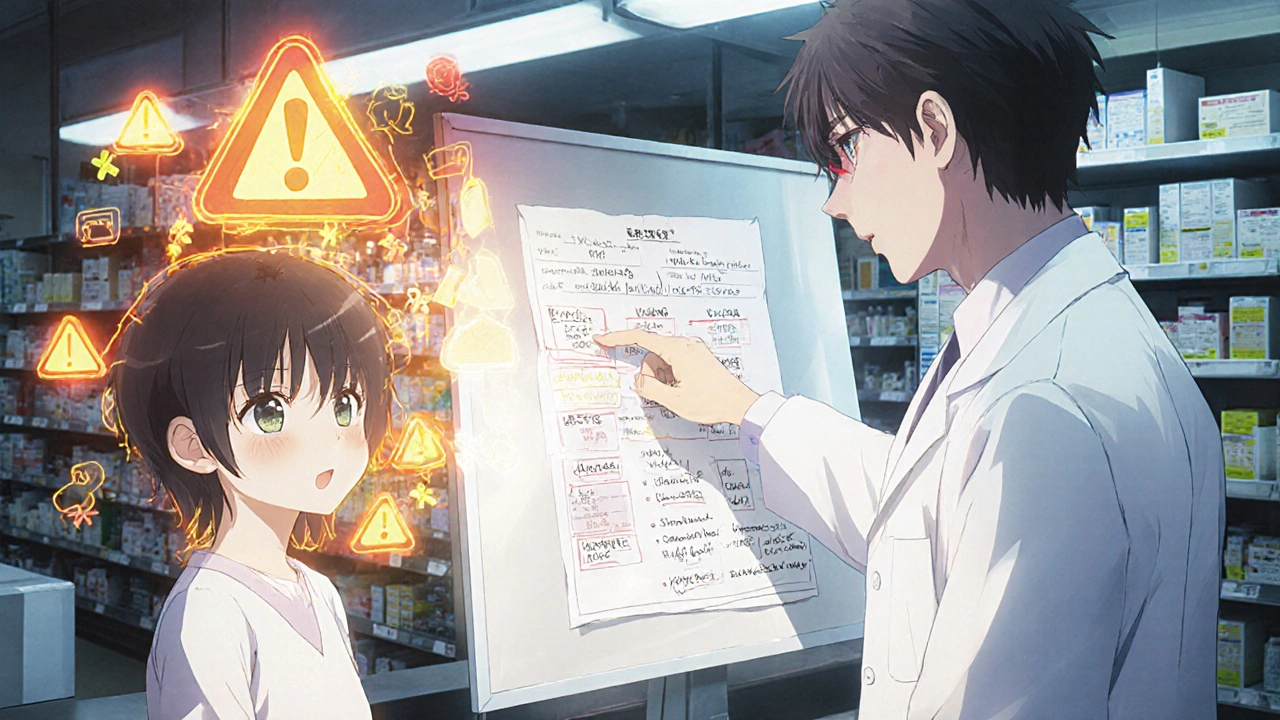
What makes a good EHR allergy system? It needs to be medication safety, the practice of preventing harmful drug reactions through accurate records and smart alerts first. That means letting you, the patient, update your own allergies with details—not just a dropdown menu. It needs to cross-check every new prescription against your history, not just the top 5 drugs. And it must connect with pharmacies so your local pharmacist sees the same alerts your doctor does. Right now, many systems don’t. A patient with a documented sulfa allergy might still get a diuretic that contains sulfa because the EHR didn’t flag it. Or worse—the system didn’t even let the doctor know the allergy was suspected, not confirmed.
The drug interactions, harmful combinations of medications that can cause serious side effects or reduce effectiveness you’re trying to avoid don’t care if your allergy record is outdated. They only care if the wrong pill gets into your body. That’s why the best EHR allergy systems don’t just store data—they use it. They alert staff when a new prescription matches your allergy profile. They remind nurses to double-check before giving a shot. They even suggest alternatives if a drug is unavoidable. And they do it fast—before the pharmacist even opens the bottle.
What you’ll find in the posts below isn’t just theory. These are real stories from pharmacists who’ve seen the gaps, patients who’ve been harmed by broken systems, and doctors who’ve fixed them. You’ll learn how to make sure your own allergy info is accurate, what to ask your provider about their EHR, and why some "allergy alerts" are useless noise while others could save your life. This isn’t about technology for tech’s sake. It’s about making sure the next time you walk into a clinic, the person handing you a prescription actually knows what could kill you—and stops it before it happens.
Learn how to interpret pharmacy allergy alerts correctly-why most are false, how to tell real risks from noise, and what steps you can take to fix inaccurate records in your health system.