If your skin flares from small changes—temperature, stress, or a new soap—you’re not alone. Atopic dermatitis (eczema) shows up as dry, itchy patches that can crack, ooze, or get infected. You don’t need perfect products; you need a routine that cuts triggers and heals the skin barrier.
Start with baths and showers. Use lukewarm water, limit time to 5–10 minutes, and skip harsh soaps. Choose a mild, fragrance-free cleanser or a soap-free wash. After you step out, pat the skin gently—don’t rub—and apply a thick moisturizer while skin is still damp. That locks in moisture better than waiting.
Pick emollients with petrolatum, mineral oil, or ceramides. Ointments and thick creams work better than lotions for itchy, cracked areas. Apply moisturizer twice daily at minimum, and more if your skin feels tight. At night, put a thicker layer on and wear soft cotton pajamas—avoid wool and scratchy fabrics.
Laundry matters. Use fragrance-free, dye-free detergents and cool or warm water. Rinse well and skip fabric softeners that leave residues that can irritate skin. Keep indoor humidity around 40–50% in dry months to stop your skin from drying out.
When a flare starts, short courses of topical corticosteroids usually calm inflammation fast. Use the strength and schedule your doctor recommends—low potency for the face and skin folds, stronger for thick areas like the palms. If steroids aren’t right for sensitive areas, prescription topical calcineurin inhibitors (like tacrolimus) are an alternative your dermatologist may suggest.
For severe or widespread cases, dermatologists can offer phototherapy, oral medicines, or newer biologic injections that target the immune response. These are for people who don’t respond to creams and moisturizers. If you’re considering prescription treatments, get a specialist’s advice.
Itch control can help you sleep and stop scratching. Non-drowsy antihistamines rarely stop itch from eczema, but a short-term sedating antihistamine at night can help break the scratch-sleep cycle. Wet-wrap therapy (moist dressing over medicated skin) can calm bad flares for a few days—ask your provider how to do it safely.
Watch for signs of infection: increased redness, warmth, pain, yellow crusting, or fever. Infections need prompt medical care and sometimes antibiotics. Also consider allergy checks if specific triggers—pets, dust mites, or foods—seem to cause clear flare patterns.
Small steps add up: gentle cleansing, aggressive moisturizing, trigger control, and clear plans for flares make eczema manageable. If your routine doesn’t help or skin gets worse, see a dermatologist — faster treatment often prevents scarring and infections.
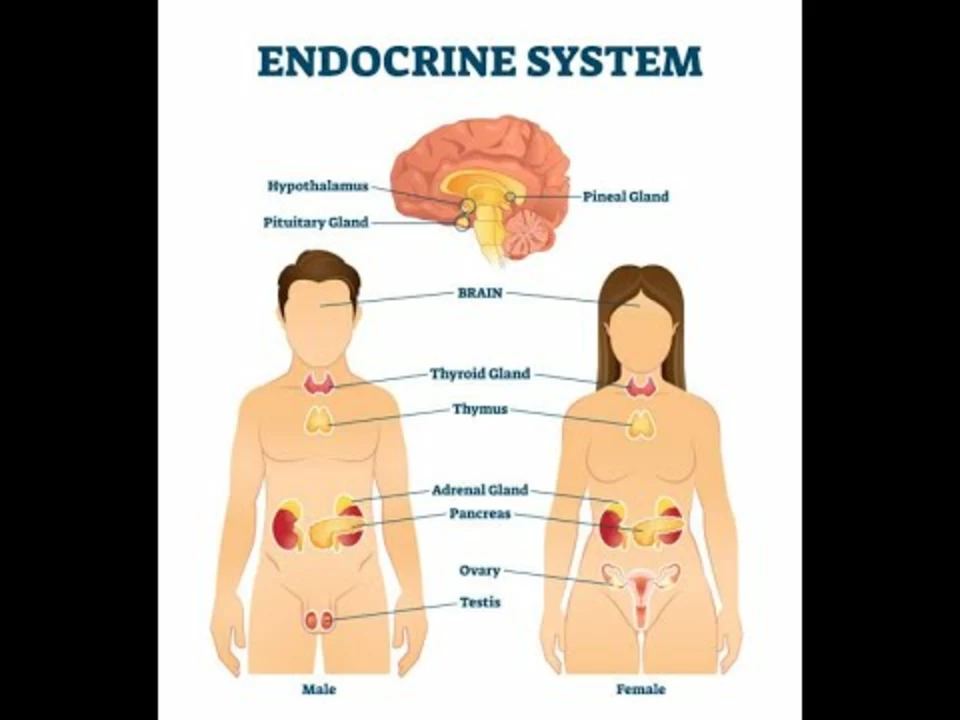
In a recent exploration of the link between hormonal imbalances and atopic dermatitis, I discovered that our hormones can play a significant role in the development and severity of this skin condition. Fluctuations in hormones, such as during pregnancy or puberty, can exacerbate atopic dermatitis symptoms. Stress, which affects our cortisol levels, can also contribute to worsening skin issues. Furthermore, individuals with thyroid disorders may experience more severe atopic dermatitis due to imbalances in their hormone production. Overall, understanding and addressing these hormonal imbalances could lead to more effective treatments and management strategies for atopic dermatitis sufferers.