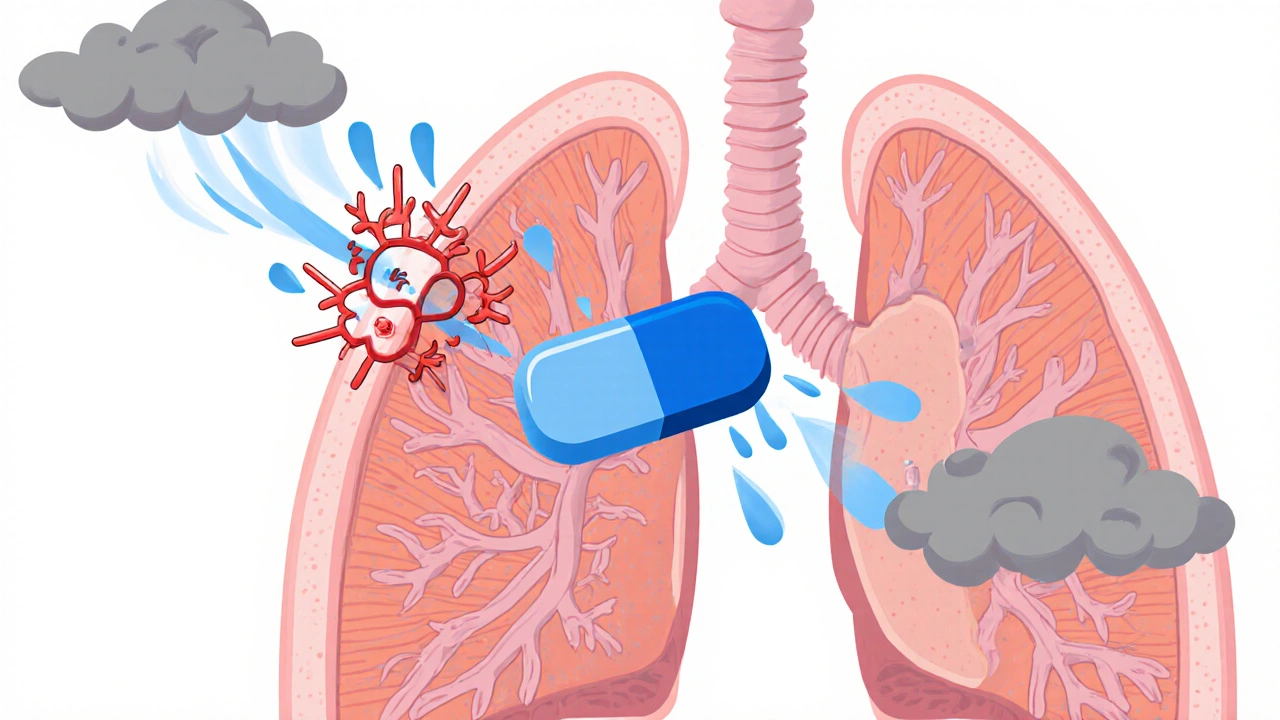
When working with asthma medication comparison, the process of weighing different drug classes to decide which best controls a patient’s symptoms. Also known as asthma drug comparison, it helps you avoid trial‑and‑error and saves time. One of the first groups you’ll encounter is inhaled corticosteroids, anti‑inflammatory powders or sprays that reduce airway swelling and prevent attacks. Right after that, bronchodilators, quick‑acting relievers that open narrowed airways by relaxing smooth muscle often show up on the comparison chart. Understanding how these two core classes work together sets the stage for a deeper dive into the full spectrum of asthma treatments.
Beyond the basics, a solid asthma medication comparison must examine the specialty agents that target specific pathways. Leukotriene modifiers, oral pills that block inflammatory chemicals called leukotrienes, are useful for patients who need an extra layer of control. Then there are the newer biologic therapies, injectable antibodies designed for severe asthma driven by specific immune triggers. Each of these options brings unique attributes: dosage frequency, cost, side‑effect profile, and the level of symptom relief they provide. For example, leukotriene modifiers are taken once daily and cost less than most biologics, while biologics may require quarterly clinic visits but can dramatically cut exacerbations in patients with high eosinophil counts. These attribute‑value pairs help you match a drug’s strengths to your personal health goals.
Putting the pieces together, an effective asthma medication comparison relies on a clear asthma action plan, a written guide that tells you when to use each medication, how to adjust doses, and when to seek emergency care. The plan links drug selection to real‑world use: inhaled corticosteroids form the daily backbone, bronchodilators act as rescue tools, leukotriene modifiers add maintenance support, and biologics serve as rescue‑escalation for severe cases. Adding peak flow monitoring, a simple at‑home test that measures airway openness, completes the feedback loop. By tracking peak flow numbers, you can see how each medication class affects lung function, turning abstract comparisons into measurable outcomes.
Armed with these definitions and relationships, you’ll be ready to explore the detailed articles below. They break down each drug class, compare efficacy, side effects, and cost, and give practical tips on how to incorporate them into your daily routine. Dive in to find the comparison that matches your lifestyle and breathing needs.
Explore a detailed comparison of Montair (montelukast) with alternative asthma drugs, covering mechanisms, side‑effects, costs and when each option works best.