Feeling mixed about antidepressants is normal. They can help a lot, but they also bring choices and trade-offs. This page gives short, useful facts so you know what to ask your doctor, how to spot side effects, and how switching usually works.
Most people start with SSRIs (like sertraline or fluoxetine). They raise serotonin and often help mood and anxiety with fewer side effects than older drugs. SNRIs (venlafaxine/Effexor, duloxetine) affect serotonin and norepinephrine — they can help pain and energy, but watch blood pressure. Tricyclics and MAOIs work too, but doctors save them for when others fail because of more risks and interactions. Atypical antidepressants (bupropion, mirtazapine) can be good if you have specific problems like low energy or sleep issues.
Expect some waiting: antidepressants usually take 4–6 weeks to show clear benefit, and dose changes can take several weeks to settle. If you feel worse in the first two weeks — more anxious or low energy — call your prescriber. Do not stop suddenly; some drugs cause withdrawal symptoms within days.
Common side effects are nausea, sleep changes, sexual issues, and mild headaches. Most ease after a few weeks. Venlafaxine (Effexor) is known for stronger withdrawal — taper slowly. If sexual side effects matter, ask about bupropion or dose timing. If you have high blood pressure, your doctor will watch it on SNRIs.
Mixing alcohol with antidepressants usually makes side effects worse and can blunt benefits. Some combos are dangerous: MAOIs interact with many foods and drugs. Always tell your provider about other meds, supplements, and herbal remedies. If you're pregnant or trying to conceive, ask for a plan — some meds are safer than others in pregnancy.
Switching meds is common. Two safe approaches are cross-tapering (slowly lowering one while raising the other) or a washout (stopping one, waiting, then starting the next). Fluoxetine needs a longer washout because it sticks around longer. Your doctor will pick the method based on the drugs involved and your symptoms.
If you take benzodiazepines and want to stop, options like buspirone can help manage anxiety longer-term. Withdrawal from benzodiazepines should also be gradual and supervised. For sleep problems, trazodone has alternatives; some are better for short-term insomnia and others for long-term use. We have deeper pieces on switching from benzodiazepines, trazodone alternatives, and detailed Effexor guidance if you want specifics.
Final practical steps: keep a symptom log, set a follow-up 4–6 weeks after starting or changing dose, and never stop abruptly. If you buy meds online, use licensed pharmacies and a valid prescription. Questions you can ask your clinician: What should I expect in the first two weeks? How will we taper if needed? Are there interactions with my other drugs? Those three questions go a long way toward safer, smarter treatment.
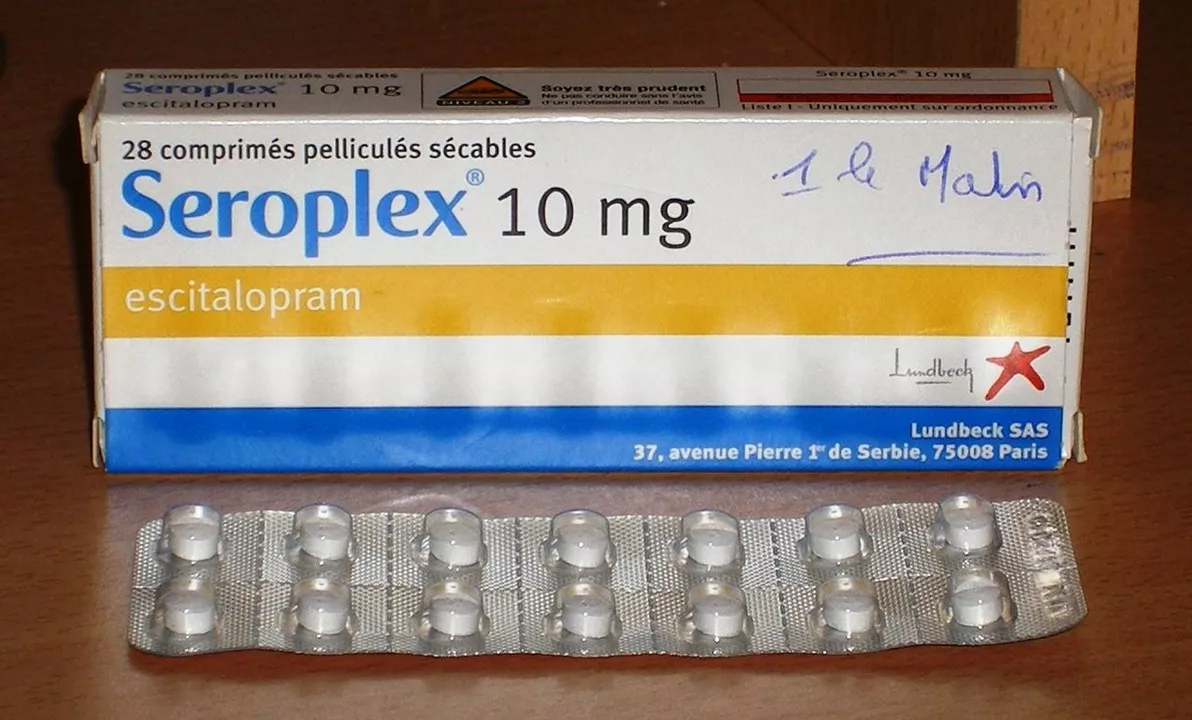
As a blogger, I've been researching the differences between Escitalopram and other antidepressants. One thing that sets Escitalopram apart is its higher selectivity for serotonin reuptake inhibition, which may lead to fewer side effects. Additionally, it has a faster onset of action, meaning it starts working more quickly than some other antidepressants. However, it's essential to remember that every individual's experience with antidepressants is unique, and what works for one person may not work for another. Nonetheless, the unique benefits of Escitalopram make it an option worth considering for those struggling with depression or anxiety.