Every night, while you sleep, your body might be fighting for air without you even knowing it. If you snore loudly, wake up gasping, or feel exhausted even after a full night’s rest, you could be one of the 1 billion adults worldwide living with obstructive sleep apnea (OSA). And what most people don’t realize is that this isn’t just a nuisance-it’s a silent killer for your heart.
How Sleep Apnea Strains Your Heart
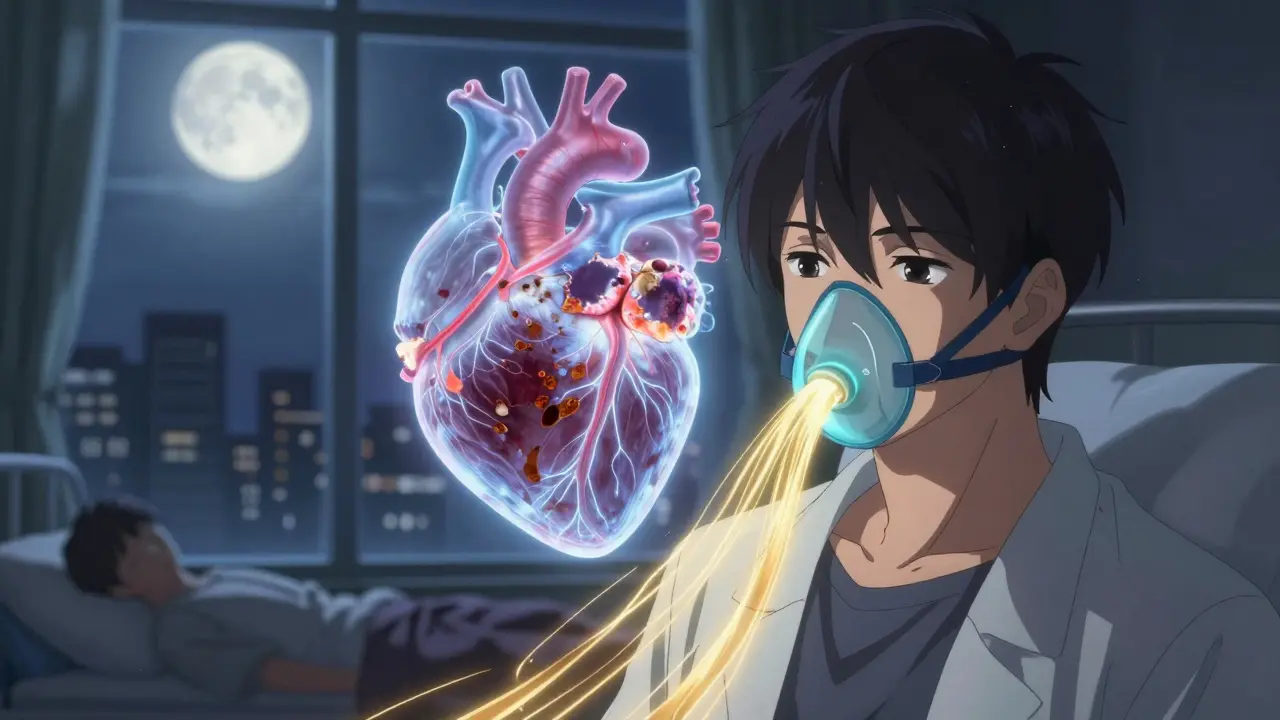
Sleep apnea isn’t just about snoring. It’s when your airway collapses repeatedly during sleep, cutting off oxygen for 10 seconds or more. Each time this happens, your brain panics. It jolts you awake-just enough to breathe, but not enough for real rest. This cycle can repeat 30, 50, even 100 times an hour.What happens inside your body during these episodes is what makes it so dangerous. Your oxygen levels drop. Your heart rate spikes. Your blood pressure surges by 20 to 40 mmHg in seconds. This isn’t a one-time spike. It happens every single night, over and over. Over months and years, that constant stress rewires your cardiovascular system.
Doctors now know that OSA doesn’t just worsen high blood pressure-it causes it. About 30 to 40% of people with high blood pressure have undiagnosed sleep apnea. And for those with resistant hypertension-blood pressure that won’t drop even with three medications-the odds jump to over 80%. The reason? Your sympathetic nervous system stays stuck in high gear. It’s like your body’s alarm system is permanently turned on.
The Link Between Sleep Apnea and Irregular Heartbeats
If you’ve ever felt your heart flutter, race, or skip a beat, you’ve experienced an arrhythmia. For people with sleep apnea, these episodes aren’t rare. Research shows they’re 3 to 5 times more common than in people who sleep normally.Atrial fibrillation (AFib)-the most common type of arrhythmia-is especially tied to OSA. While high blood pressure raises AFib risk by about 50%, severe sleep apnea increases it by 140%. Why? Each time your oxygen drops, your heart’s electrical system gets thrown off. Vagal nerves slow your heart. Then, as you gasp for air, your sympathetic system fires like a rocket. That back-and-forth chaos creates perfect conditions for erratic rhythms.
Studies using cardiac MRI now show that people with untreated OSA have 2.3 times more scarring (fibrosis) in their upper heart chambers. That scar tissue doesn’t conduct electricity properly. It’s like rust on wires-messing up the signals that keep your heartbeat steady. And once that scarring sets in, even treating the sleep apnea later won’t fully undo the damage.
Why OSA Is Worse Than You Think
Some people think if they’re young, fit, or not overweight, they’re safe. That’s a dangerous myth. A major 2024 study from UT Southwestern Medical Center found that OSA increases heart risk even in adults under 40. You don’t need to be obese. You don’t need to be old. Just having frequent breathing pauses during sleep is enough to start damaging your heart.And it’s not just about heart rhythm. OSA raises your risk of stroke by 60%, heart failure by 140%, and coronary artery disease by 30%. These aren’t small numbers. They’re bigger than the risk from high cholesterol in some cases. What makes OSA so insidious is that it works behind the scenes. You might feel fine during the day. Your cholesterol looks good. Your weight is normal. But inside, your heart is being battered night after night.
How CPAP Therapy Can Reverse the Damage
The good news? This damage isn’t permanent-if you act. Continuous Positive Airway Pressure (CPAP) therapy is the most studied and effective treatment. It’s a machine that delivers gentle air pressure through a mask, keeping your airway open while you sleep.Consistent use-4 or more hours a night-can lower systolic blood pressure by 5 to 10 mmHg on average. That’s the same drop you’d get from a low-dose blood pressure pill. For people with atrial fibrillation, CPAP reduces recurrence by 42% after just 12 months. One user on the American Heart Association’s forum shared that after six months of CPAP, his AFib episodes dropped from weekly to once every two months.
And it’s not just about numbers. People report real changes: less morning headaches, more energy, better focus. A 2024 survey of over 5,000 CPAP users found that 65% were able to reduce their blood pressure medication, and 78% said their daytime tiredness improved dramatically.
What Stops People From Using CPAP
The biggest problem isn’t the machine-it’s the habit. About 25 to 30% of people stop using CPAP within the first year. Why? Mask discomfort, dry mouth, claustrophobia, or just forgetting to wear it.But most of these issues have fixes. Try a nasal pillow mask if the full-face one feels too bulky. Use a humidifier attachment to stop dryness. Turn on the “ramp” feature so the pressure starts low and builds slowly. Replace the mask cushion every three months-it gets stiff and leaks over time.
It takes about 2 to 4 weeks to adjust. Most people who stick with it for 30 days say their sleep quality improves noticeably. The key isn’t perfection-it’s consistency. Even 3 nights a week helps. But 5 or more nights? That’s when the heart starts healing.
Who Should Get Tested
You don’t need to wait for symptoms to get worse. If you have any of these, get screened:- High blood pressure, especially if it’s hard to control
- Atrial fibrillation or other irregular heart rhythms
- History of stroke or heart failure
- Snoring loudly, with pauses in breathing
- Waking up gasping or choking
- Constant daytime fatigue, even after 8 hours of sleep
Doctors now recommend screening for all of these groups. In fact, 45 to 65% of people with heart conditions like AFib or heart failure have undiagnosed sleep apnea. Yet, only 20 to 25% of at-risk patients are even tested.
Testing is easier than ever. Most people can do a home sleep test-wear a small device overnight, send it back, and get results in a week. No hospital stay. No needles. Just a simple, non-invasive way to find out if your heart is at risk.
The Bigger Picture
The global market for sleep apnea devices is expected to hit $14.7 billion by 2028. Why? Because more doctors and patients are waking up to the connection. Medicare and private insurers now cover testing and treatment for people with heart conditions. The American Heart Association officially lists OSA as a Class I risk factor for arrhythmias-on the same level as obesity and hypertension.What’s changing is the mindset. Sleep apnea isn’t just a sleep problem. It’s a heart problem. And treating it isn’t optional-it’s essential for long-term heart health.
If you’ve been told you snore, or you’re tired all the time, or your blood pressure won’t budge-don’t ignore it. Ask your doctor for a sleep test. It could be the simplest, most life-saving step you take this year.
Can sleep apnea cause high blood pressure even if I’m not overweight?
Yes. While obesity increases the risk of sleep apnea, it’s not required. People with normal weight can still have narrow airways, jaw structure issues, or muscle tone problems that cause breathing pauses. The mechanical stress from repeated oxygen drops directly triggers blood pressure spikes, regardless of body weight. Studies show 30-40% of people with high blood pressure have untreated sleep apnea-even if they’re lean.
Does treating sleep apnea reduce the need for heart medications?
Many patients find yes. In a 2024 survey of over 5,200 CPAP users, 65% reported needing fewer blood pressure medications after consistent therapy. CPAP lowers nighttime blood pressure spikes, which reduces overall strain on the heart and blood vessels. For some, this means lower doses. For others, it means dropping a medication entirely. Always work with your doctor before making changes.
Is sleep apnea linked to atrial fibrillation in younger people?
Absolutely. A 2024 study from UT Southwestern Medical Center found that obstructive sleep apnea increases atrial fibrillation risk even in adults under 40. Previously, doctors thought this was mostly an older adult issue. Now we know that the repetitive oxygen drops and heart stress from OSA can start damaging the heart’s electrical system at any age. Early diagnosis and treatment can prevent long-term rhythm problems.
How long does it take for CPAP to improve heart health?
Some benefits start within weeks. Blood pressure often drops within the first month of consistent use (4+ hours/night). For arrhythmias like atrial fibrillation, studies show a 42% reduction in episodes after 12 months of regular therapy. The longer you use CPAP, the more your heart recovers-reducing inflammation, improving oxygen delivery, and stabilizing heart rhythms over time.
What if I can’t tolerate CPAP?
There are alternatives. Oral appliances that reposition the jaw can help mild to moderate cases. Positional therapy (sleeping on your side) reduces apneas for some. For severe cases that don’t respond to CPAP, a newer option called Inspire Therapy-a small implanted device that stimulates the nerve controlling the tongue-has shown 79% reduction in breathing pauses. Talk to a sleep specialist about your options.
Can I test for sleep apnea at home?
Yes. Home sleep apnea tests are now standard for most people. You’ll wear a small device on your finger, chest, and nose overnight. It tracks breathing, oxygen levels, and heart rate. After sending it back, results are reviewed by a sleep specialist. These tests are accurate for detecting obstructive sleep apnea in 80% of cases and are covered by most insurance plans, especially if you have heart-related symptoms.
Is central sleep apnea as dangerous as obstructive sleep apnea for the heart?
Not as much. Central sleep apnea, where the brain fails to signal the lungs to breathe, is less common and usually linked to heart failure or stroke. While it still affects heart rhythm, it doesn’t cause the same intense pressure swings or oxygen drops as obstructive sleep apnea. Obstructive sleep apnea is the main driver of high blood pressure, arrhythmias, and heart damage. Most screening and treatment focuses on OSA.
If you’ve been told you snore, or you’re tired all the time, or your blood pressure won’t budge-don’t ignore it. Ask your doctor for a sleep test. It could be the simplest, most life-saving step you take this year.

Aditya Kumar
December 15 2025Man, I snore like a chainsaw but I just blame it on being tired. Guess I’m one of those billion people who don’t wanna face it.