When your kidneys aren't draining properly, time matters. A blocked ureter, a swollen renal pelvis, or a kidney that’s shrinking over time can slip past notice until damage is done. That’s where renal ultrasound comes in - not as a fancy last resort, but as the first, safest, and most practical step to find out what’s really going on inside your kidneys.
Why Ultrasound Is the First Test for Kidney Problems
You’ve probably heard of CT scans for kidney stones. They show everything - down to a 1-mm speck of stone. But they also expose you to radiation, sometimes the equivalent of 3-5 years of natural background exposure. For someone with recurrent kidney issues, that adds up fast. Enter renal ultrasound: no radiation, no needles, no contrast dye. Just sound waves bouncing off your kidneys to paint a real-time picture. It’s not just safer - it’s faster. In emergency rooms across Australia and the U.S., point-of-care ultrasound cuts diagnosis time for suspected kidney obstruction by nearly an hour. A patient walks in with sharp flank pain, and within minutes, the doctor can see if the kidney is swollen with backed-up urine - a sign called hydronephrosis. That’s enough to start treatment before waiting for a formal scan. Major guidelines from the Cleveland Clinic, Mayo Clinic, and the American College of Emergency Physicians all agree: if you suspect obstruction, start with ultrasound. It’s cheaper, quicker, and avoids unnecessary radiation. Especially in kids, pregnant women, or people needing repeated scans, it’s the only sensible first move.What Ultrasound Actually Measures
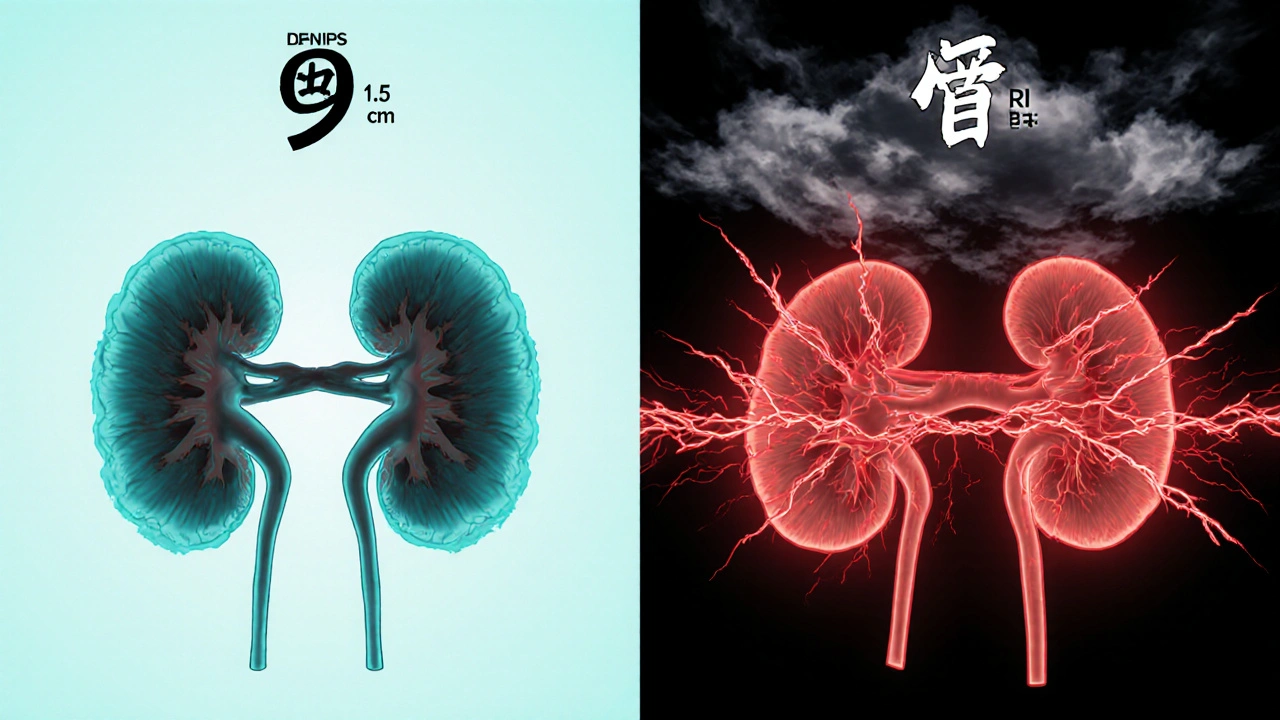
A renal ultrasound isn’t just a picture. It’s a set of measurements. The sonographer doesn’t just look - they measure.- Kidney length: Normal adult kidneys are 9 to 13 centimeters long. If one is 7 cm, it’s likely scarred or chronically damaged.
- Cortical thickness: The outer layer of the kidney should be at least 1 cm thick. Thinning means long-term pressure or disease is eating away at the working tissue.
- Renal pelvis diameter: The central collecting area should be less than 7 mm wide. Anything bigger suggests urine is backing up.
- Resistive index (RI): This is where ultrasound gets smart. It measures how easily blood flows through the kidney’s small arteries. A normal RI is below 0.70. Above that? It’s a red flag. A 2015 study showed an RI of 0.70 or higher detects obstruction with 87% accuracy. It’s not perfect, but it’s a powerful clue.
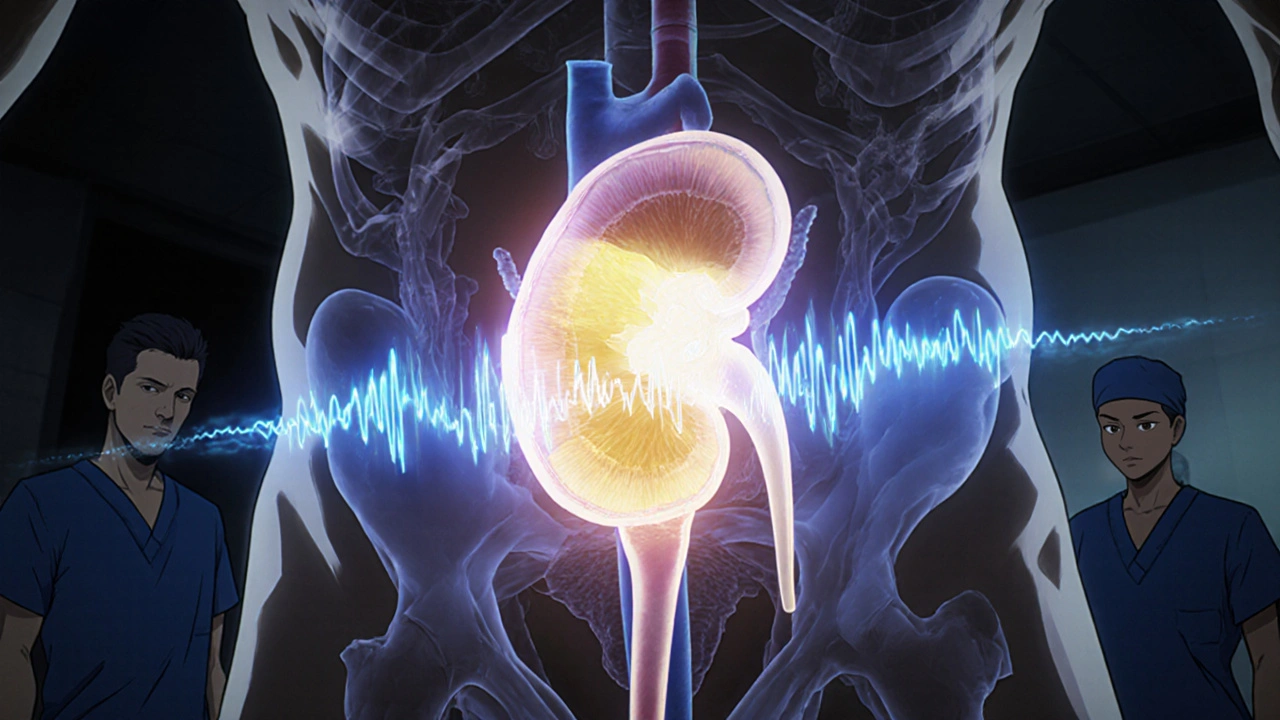
Hydronephrosis: The Telltale Sign of Blockage
Hydronephrosis isn’t a disease. It’s a sign - the swelling you see when urine can’t leave the kidney. Ultrasound grades it from mild to severe using the Society for Fetal Urology scale:- Mild: Only the renal pelvis is slightly widened.
- Moderate: The pelvis and some calyces (the tiny cups inside the kidney) are dilated.
- Severe: The entire kidney looks ballooned, the cortex is thinning, and the organ is losing its normal shape.
Doppler and Elastography: The New Tools Making Ultrasound Smarter
Ultrasound isn’t stuck in the 1980s. Modern machines now use Doppler to map blood flow patterns and shear-wave elastography to measure how stiff the kidney tissue is. When a kidney is blocked, pressure builds. That pressure squeezes the tiny blood vessels inside. Doppler picks up the resistance - that’s the RI we talked about. But now, elastography goes further. It literally feels the kidney. Think of it like pressing on a water balloon. The more pressure inside, the firmer it gets. Studies show that as obstruction worsens, kidney stiffness increases in a straight line. This isn’t just theory - it’s being used in research hospitals to track how well a patient responds to treatment. Even more exciting? Super-resolution ultrasound. New techniques can now visualize blood vessels so small they were invisible before. This could let doctors spot early signs of scarring - long before kidney function drops. It’s still experimental, but it’s the future.Where Ultrasound Falls Short
Let’s be clear: ultrasound isn’t magic. It has limits.- Small stones: It misses about 20% of stones under 3 mm. If you’re in severe pain and the ultrasound looks normal, don’t assume you’re fine. A CT might still be needed.
- Obese patients: If your BMI is over 35, sound waves can’t penetrate deep enough. The image gets blurry. That’s when you switch to MRI or CT.
- No function data: Ultrasound shows structure - not how well the kidney is working. It can’t tell you if one kidney is producing 10% of urine and the other 90%. For that, you need a nuclear scan - but that involves radiation.
- Operator skill matters: A 2018 study found up to 20% variation in kidney size measurements between inexperienced and expert sonographers. That’s why training is critical. The American Institute of Ultrasound in Medicine requires 40 supervised exams before you’re certified.
Ultrasound vs. CT vs. MRI: What’s Best When?
Here’s a simple guide to choosing the right test:| Feature | Renal Ultrasound | CT Urography | Magnetic Resonance Urography (MRU) |
|---|---|---|---|
| Radiation | None | High (10 mSv per scan) | None |
| Cost (USD) | $200-$500 | $800-$1,500 | $1,500-$2,500 |
| Stone detection | 80% of stones >3 mm | 99% of stones >1 mm | Poor - misses most stones |
| Hydronephrosis detection | Excellent | Excellent | Excellent |
| Functional data | Yes, with Doppler | Yes, with contrast timing | Yes, with dynamic imaging |
| Best for | First-line, kids, pregnancy, follow-up | Complex cases, small stones, emergency | Contrast allergy, detailed anatomy, no radiation needed |
What Happens After the Scan?
If your ultrasound shows mild hydronephrosis and no stone, you might just be told to drink water and come back in a few weeks. No rush. But if it shows severe swelling, a thin cortex, and a high resistive index? That’s a red flag. You’ll likely be referred to a urologist. They’ll want to know:- Is the blockage in the ureter? The ureteropelvic junction? The bladder?
- Is it caused by a stone, a tumor, or a congenital twist?
- Is the kidney still working, or is it already damaged?
What’s Next for Renal Ultrasound?
The future isn’t about bigger machines. It’s about smarter analysis. Hospitals are now testing AI that can automatically measure kidney size and grade hydronephrosis - removing human error. One Mayo Clinic trial showed AI matching expert radiologists in accuracy, but doing it in seconds instead of minutes. Meanwhile, researchers are exploring ultrasound localization microscopy - a technique that could one day count individual nephrons, the kidney’s filtering units. Imagine being able to see how many filters are still working, without a biopsy. These aren’t sci-fi dreams. They’re happening now. And they’re all built on the same foundation: ultrasound’s safety, accessibility, and ability to be repeated.Final Thoughts: Trust the Basics
In a world obsessed with high-tech scans and flashy diagnostics, it’s easy to forget the power of the simple. Renal ultrasound doesn’t need a fancy lab or a radioactive tracer. It just needs a trained hand and a good machine. It’s the first test because it’s the right test. It answers the big questions: Is the kidney swollen? Is it shrinking? Is blood flow restricted? Is something blocking the flow? If you’re being evaluated for kidney pain, ask: “Can we start with an ultrasound?” If the answer is no - push back. You’re not just avoiding radiation. You’re choosing a smarter, safer path to diagnosis.Can a renal ultrasound detect kidney stones?
Yes, but not all of them. Renal ultrasound detects about 80% of kidney stones larger than 3 mm. Smaller stones, especially under 2 mm, often go unseen. If your symptoms are strong but the ultrasound is normal, a CT scan may still be needed to rule out tiny stones or other causes of obstruction.
Is renal ultrasound safe during pregnancy?
Yes, it’s the preferred imaging method during pregnancy. Unlike CT or X-rays, ultrasound uses no radiation and no contrast agents. It’s routinely used to check for hydronephrosis in pregnant women, which is common due to hormonal changes and pressure from the growing uterus.
What does a high resistive index mean?
A resistive index (RI) above 0.70 suggests increased resistance to blood flow in the kidney, often caused by obstruction, scarring, or high pressure inside the kidney. It’s not a diagnosis on its own, but when combined with hydronephrosis and kidney size, it strongly points to a blockage or chronic damage. Studies show it’s 87% accurate in detecting obstructive uropathy.
Can obesity affect the results of a renal ultrasound?
Yes. In patients with a BMI over 35, sound waves struggle to penetrate deep enough to get clear images of the kidneys. This can make it hard to measure kidney size, detect small stones, or assess the renal pelvis accurately. In these cases, doctors often turn to CT or MRI instead.
How often should someone with a history of kidney obstruction get an ultrasound?
There’s no fixed schedule - it depends on the cause and severity. After surgery for a ureteropelvic junction (UPJ) obstruction, patients often get weekly ultrasounds for the first month, then monthly for three months, then every 3-6 months for a year. For chronic conditions like recurrent stones, ultrasounds may be done every 6-12 months to monitor kidney size and check for new blockages. The goal is to avoid radiation while catching problems early.
Do I need to prepare for a renal ultrasound?
Usually, no special prep is needed. You don’t have to fast. But being well-hydrated helps - a full bladder pushes bowel gas out of the way and gives a clearer view of the kidneys and ureters. Your provider may ask you to drink 1-2 glasses of water an hour before the scan and not urinate until after.
Renal ultrasound is not just a tool - it’s a strategy. It’s how you protect your kidneys without harming your body. And in a world full of complex, costly, and risky tests, that’s worth remembering.

David Cunningham
November 24 2025Been using point-of-care US in the ER here in Sydney for years. Cut our time-to-diagnosis way down. No radiation, no waiting. Just slap the probe on and know if it's hydronephrosis or not. Game changer.