PMI Knowledge Check
How Much Do You Know About the FDA's PMI Changes?
This quiz tests your knowledge of the new Patient Medication Information (PMI) requirements. Answer the questions below to see how well you understand this important change to medication labeling.
Question 1
What is the FIRST line of text that MUST appear on every Patient Medication Information (PMI)?
Question 2
Which of the following information MUST be included on every PMI?
Question 3
What is the FDA's primary reason for requiring standardized PMIs?
Question 4
Which of the following is TRUE about electronic PMIs?
Question 5
What is a key criticism of the current PMI draft?
The U.S. Food and Drug Administration (FDA) is pushing forward with a major overhaul of how patients receive information about their prescription drugs. Right now, most people get a small paper insert or a label on the bottle with basic directions. But starting in 2025, that could change - dramatically. The FDA’s proposed Patient Medication Information (PMI) rule would require every outpatient prescription drug to come with a single-page, standardized information sheet designed to be clear, consistent, and easy to understand. This isn’t a minor tweak. It’s the biggest shift in medication labeling in decades.
What Exactly Is the PMI?
The PMI is meant to replace the current patchwork of Medication Guides, which are only required for about 150 out of thousands of prescription drugs - mostly those with serious risks like opioids or blood thinners. Under the new rule, every prescription you pick up at the pharmacy - from antibiotics to antidepressants - would come with a PMI. It would look the same no matter where you go: CVS, Walgreens, or your local independent pharmacy. The goal? Reduce confusion and prevent mistakes that lead to injuries or death.
The FDA estimates that medication errors cause 1.3 million injuries and 7,000 deaths each year in the U.S. Many of these happen because patients don’t understand how to take their medicine. The current labels often focus on insurance codes, pharmacy phone numbers, or expiration dates - not what matters most: how to use the drug safely. The PMI flips that. It starts with a bold statement: “Use exactly as prescribed.” Then it gets straight to the point.
What’s on the PMI?
The format is strict. Every PMI must follow the same structure:
- Heading: “Patient Medication Information”
- First line: “Use exactly as prescribed”
- Directions for use: How to take it - with meals? At night? Can you crush it?
- Storage: Keep at room temperature? Refrigerate? Keep away from children?
- Disposal: How to safely get rid of leftover pills
- Warnings: What to avoid - alcohol, driving, other drugs
- Common side effects: What to expect - nausea, dizziness, fatigue
It’s all written in plain language, at a 12-point font, using simple words. No jargon. No marketing. No fluff. The FDA tested dozens of versions with real patients. Those with limited health literacy understood the new format 25-40% better than current guides. That’s huge. About 80 million U.S. adults struggle to understand health information. The PMI was built for them.
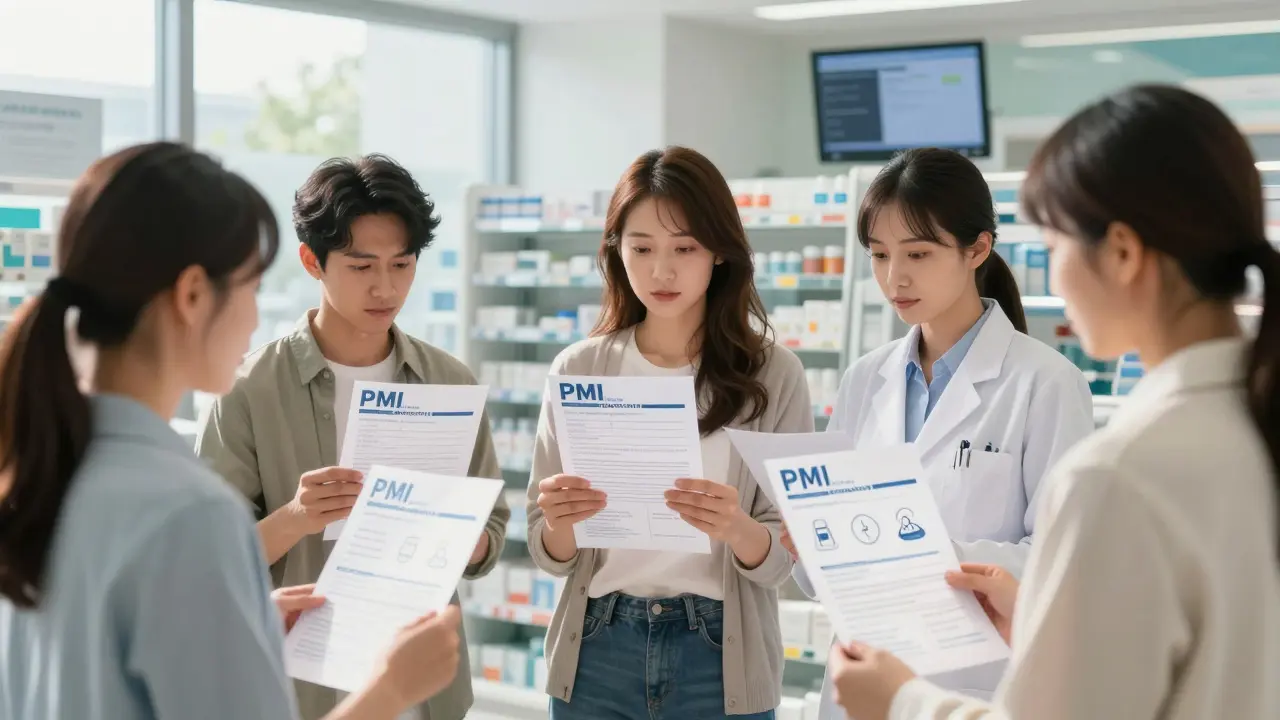
Electronic PMI? Yes - But Paper Still Required
The FDA knows not everyone wants paper. So, you’ll also be able to get your PMI electronically - through a pharmacy app, email, or a secure patient portal. But here’s the catch: pharmacies must still offer a printed copy if you ask for it. No one gets left behind. This is a key part of the rule. Accessibility isn’t optional. Digital versions must meet Section 508 standards - meaning screen readers, large text options, and simple navigation are required.
What’s Missing? A Big Debate
While the PMI is a step forward, it’s not perfect. Researchers at the University of Pittsburgh took the FDA’s template and built their own version - called “Decision Critical PMI.” Their version didn’t just say “common side effects.” It gave numbers: “48% of patients experience fever. 43% get a headache.” That kind of detail helps patients weigh risks. Should you take this drug if you’re worried about fever? With the FDA’s version, you’re left guessing.
And there’s another gap: no mention of benefits. The PMI tells you how to take the drug and what might go wrong - but not why you’re taking it. What does this medication actually do? Does it reduce your chance of a stroke by 30%? Cut your pain by half? The FDA says that information should come from your doctor. But what if you forget? What if you’re seeing a new provider? What if you’re reading the PMI because your doctor didn’t explain it well?
Some experts argue this omission could hurt decision-making. If patients don’t understand the benefit, they may skip their meds - especially if side effects are scary. The FDA is aware of this. In public meetings, they’ve hinted that future updates might include benefit data. But for now, it’s not in the draft.
Who Pays for This?
Pharmaceutical companies will have to write, design, and submit a PMI for every single outpatient drug they make. That could mean tens of thousands of documents. The FDA says it will provide templates and review teams to help. But the cost is real. Industry analysts estimate this change will cost over $1.2 billion in the first five years. Most of that - 65% - falls on drugmakers. Pharmacies will spend another 25% updating systems and training staff. Each prescription may take 30-60 seconds longer to fill at first. That adds up.
Independent pharmacies are worried. About 15% of them might struggle to afford the changes without financial help, according to the National Community Pharmacists Association. The FDA hasn’t offered subsidies. That could mean delays or uneven rollout in rural or low-income areas.
How Will It Be Rolled Out?
The rule isn’t final yet. Public comments closed in late 2023. The FDA is reviewing about 1,200 submissions from patients, doctors, pharmacists, and drug companies. A final rule is expected in mid-2024. Then comes the clock:
- Large manufacturers: Must comply within 24 months
- Smaller companies: Have 36 months
- Pharmacies: Must begin distributing PMIs as soon as the rule takes effect
Training for pharmacists? About 2-4 hours per person. Annual refreshers? One hour. That’s not a lot - but it’s time they didn’t have before.
Why This Matters
This isn’t just about paperwork. It’s about safety. Patients who get clear medication instructions are 30% more likely to take their drugs correctly, according to a 2018 study. Better adherence means fewer hospital visits, fewer overdoses, fewer deaths. The National Patient Safety Foundation estimates this single change could prevent 30% of the 770,000 medication errors that happen each year outside hospitals.
It also brings the U.S. in line with global trends. The European Medicines Agency is studying a similar system for 2025. Countries like Canada and Australia already have standardized patient leaflets. The U.S. is late - but now it’s catching up.
What Comes Next?
The PMI is just the beginning. The FDA has signaled it may expand the format later to include:
- Quantified benefit data (e.g., “This drug reduces heart attack risk by 25%”)
- Drug mechanism of action (e.g., “This works by blocking a brain chemical that causes pain”)
- Interactions with common foods or supplements
For now, the focus is on safety and clarity. If the rollout goes smoothly, the PMI could become the gold standard for patient communication worldwide. If it’s poorly funded or confusing to implement, it could become another bureaucratic burden that doesn’t change behavior.
One thing is certain: if you take prescription drugs, you’ll see this change soon. And whether you get it on paper or on your phone, the goal is simple - help you use your medicine safely, without guesswork.

Tatiana Barbosa
February 7 2026This is HUGE. Finally something that makes sense. I’ve had patients ask me if they can take their blood pressure med with coffee because the tiny print said 'take with water' - no one told them what 'with water' even meant. PMI is long overdue. Let’s hope they stick to plain language and don’t let pharma water it down.