Why Generic Medication Errors Are More Common Than You Think
Generics make up 90% of all prescriptions filled in the U.S., and they save patients and insurers billions every year. But behind that efficiency is a quiet risk: generic medication errors. These aren’t just mistakes in dosage or labeling-they’re often caused by subtle differences that patients and even pharmacists don’t notice until something goes wrong.
Imagine a patient who’s been taking a white, oval pill for high blood pressure for years. One day, the pharmacy gives them a blue, round pill instead. Same name, same active ingredient. But the shape, color, and even the imprint changed. The patient thinks it’s a different drug. They stop taking it. Their blood pressure spikes. That’s not a rare scenario. It happens more often than you’d expect.
These errors aren’t always the pharmacist’s fault. Often, they’re built into the system. Multiple manufacturers produce the same generic drug, each with different looks, sizes, and inactive ingredients. One batch might contain lactose; another might not. For patients with allergies or sensitivities, that’s a problem. And if the electronic system doesn’t flag the change, no one notices until the patient walks in with complaints.
The Hidden Risks of Look-Alike and Sound-Alike Generics
One of the biggest dangers with generics is how similar their names and appearances can be. Take hydroxyzine and hydralazine. One treats anxiety. The other treats high blood pressure. They sound almost identical. If a pharmacist misreads the script-or if the computer auto-fills the wrong one-it’s easy to give the wrong drug.
It’s not just names. Some generics look so much like brand-name drugs that patients assume they’re the same. A patient might be handed a generic version of Lipitor that’s shaped and colored exactly like the brand. They think it’s the same pill, so they don’t ask questions. But if the generic switches manufacturers, the next refill might look completely different. That confusion leads to missed doses, overdoses, or patients refusing to take their meds altogether.
Studies show that 35% of preventable adverse drug events come from poor drug information. More than half of those happen at the prescribing stage. Doctors don’t always know which generic manufacturer their patient is on. They don’t know if the new batch has a different filler that could cause a reaction. And when they write the script, they often just write the generic name-no manufacturer, no formulation details.
How Technology Can Stop Errors Before They Happen
The best defense against generic errors isn’t more staff or longer hours-it’s better technology. Computerized Physician Order Entry (CPOE) systems cut medication errors by 55% in hospitals. In primary care, that number is still 48%. But most community pharmacies don’t use these systems yet. Only about 35-40% of them have integrated digital order systems that flag potential issues.
Bar code scanning at the counter is another game-changer. When a pharmacist scans the prescription and then the bottle, the system checks: Is this the right drug? The right strength? The right patient? If there’s a mismatch, it stops the process. Hospitals that use this system cut adverse drug events by half. Community pharmacies should too.
Clinical Decision Support Systems (CDSS) are even smarter. They don’t just check for dosage errors. They can flag if a patient is getting two generics with the same active ingredient. They can warn if a new generic has a different inactive ingredient that might interact with another drug the patient is taking. One case from the AHRQ showed a patient was prescribed a drug twice daily-but the label said twice weekly. The CDSS would have caught that. But only 28% of community pharmacies track errors formally. Most don’t even have the tools to catch them.
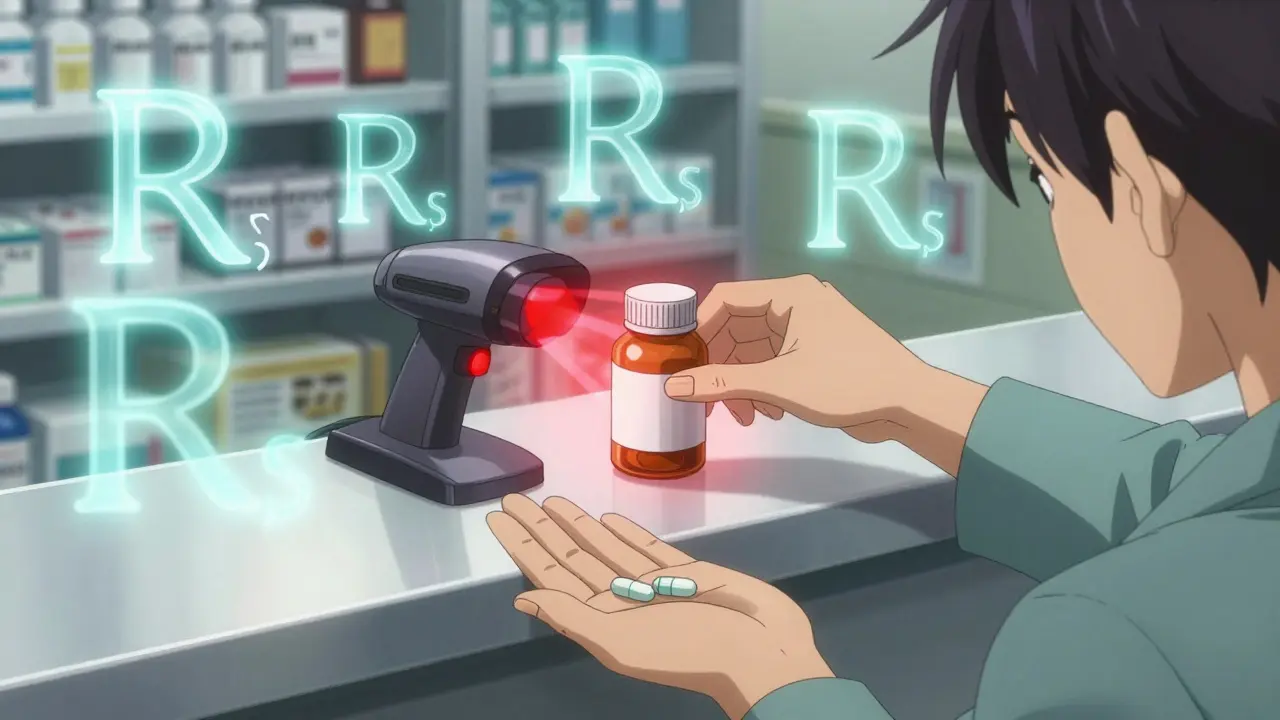
The 8 R’s: A Simple Framework That Actually Works
Even without fancy software, pharmacists can reduce errors using a tried-and-true method: the 8 R’s of medication safety.
- Right patient - Confirm identity with two identifiers, not just a name.
- Right drug - Double-check the generic name and manufacturer.
- Right dose - Verify strength, especially if the generic has changed.
- Right route - Is this supposed to be swallowed, injected, or applied topically?
- Right time - Twice daily? Twice weekly? Don’t assume.
- Right documentation - Record every change, every substitution.
- Right reason - Why is this drug being given? Is it still needed?
- Right response - Follow up. Did the patient feel better? Any side effects?
Training staff on the 8 R’s takes 8 to 12 hours. It’s not a quick fix, but it’s one of the most effective ways to reduce human error. And it doesn’t cost a dime.
Why Patient Counseling Is Your Last Line of Defense
Pharmacists are often the last person to catch an error before it reaches the patient. That’s why counseling on first fills is so critical. In high-volume pharmacies, this step gets rushed. But when done right, it catches 12-15% of potential problems.
Here’s what effective counseling looks like: “This is the generic version of your blood pressure pill. It’s the same active ingredient, but it looks different because it’s made by a different company. Some people notice a slight change in how it works, but it’s not the drug changing-just the shape or color. If you feel dizzy, nauseous, or if your blood pressure feels off, call us.”
That conversation takes 3 to 5 minutes. It’s not optional. It’s essential. And it’s especially important when switching between generic manufacturers. Patients don’t understand bioequivalence. They don’t know that a drug can be 80-125% as absorbed as the brand and still be approved. All they know is: “This pill looks different. Is it safe?”
Reddit threads from pharmacists show this is a daily issue. Patients come in angry because their new generic is a different color. They think they’ve been given the wrong medicine. A quick explanation can turn frustration into trust.

What’s Missing: Poor Tracking and Outdated Databases
Here’s the dirty secret: most pharmacy systems don’t keep good records of generic changes. Forty-two percent of pharmacists say their drug databases have outdated information on manufacturer formulations. That means when a new generic comes in, the system might still list the old inactive ingredients. Or worse-it doesn’t list them at all.
Drug references like Drug Facts and Comparisons are updated annually. But many pharmacies don’t subscribe. They rely on free apps or outdated printouts. That’s like driving with a map from 2010. It might get you there-but you’ll miss the detours.
And error reporting? Only 28% of community pharmacies track errors formally. Without data, you can’t improve. You can’t spot trends. You can’t train staff on what’s going wrong. If you don’t know how many times you’ve dispensed the wrong generic version, you’ll keep doing it.
What’s Changing: New Rules and Better Tools
Things are starting to shift. The FDA’s 2022 GDUFA III rules now require manufacturers to notify prescribers and pharmacies when they change a generic’s formulation. That’s a big step. It means if your pill suddenly turns from white to blue, the pharmacy should know why.
The WHO updated its guidelines in 2023 to push for standardized naming of generics to cut down on look-alike/sound-alike mix-ups. And the Leapfrog Group updated its hospital safety standards in early 2023 to include tracking generic substitutions across care settings. That pressure is starting to move into community pharmacies too.
Next up? AI-powered systems that predict which patients are at risk of reacting to a new generic based on their genetics. Pilot programs are already showing a 22% drop in errors beyond standard systems. It’s not science fiction-it’s coming.
What You Can Do Today
You don’t need a $75,000 software upgrade to make a difference. Start here:
- Update your drug references - Use a reliable, current source. Pay for it if you have to.
- Implement the 8 R’s - Train every staff member. Make it part of your daily routine.
- Counsel on first fills - Don’t skip it. Even if you’re busy.
- Ask patients - “Have you noticed any changes in how your medicine works lately?”
- Track your errors - Start a simple log. What went wrong? How? Could it be prevented?
Generics are safe. They’re effective. But safety isn’t automatic. It’s built-by people, by systems, by habits. The next time you hand a patient a new generic, don’t just assume they know it’s the same. Ask. Explain. Confirm. That’s how you stop an error before it starts.


Prajwal Manjunath Shanthappa
February 4 2026Let’s be real-this whole ‘generic’ paradigm is a regulatory farce. We’re told they’re ‘bioequivalent,’ but 80-125% absorption? That’s not equivalence-that’s a fucking lottery. And don’t get me started on the ‘inactive ingredients’-lactose, dyes, fillers-hidden like landmines in a pill. The FDA’s ‘GDUFA III’? A PR stunt. They don’t audit manufacturers-they just collect fees. And pharmacists? They’re just order-takers with a white coat. We need mandatory genetic screening before dispensing generics. Or at least, a damn blood test. This isn’t healthcare-it’s pharmaceutical Russian roulette.