Perioral dermatitis isn’t just a rash. It’s a frustrating, often invisible cycle of red bumps, burning skin, and the constant worry that your face is breaking out - again. And no matter how many creams you try, it won’t go away. If you’ve been told it’s acne, but your skin doesn’t have blackheads or whiteheads, and the redness circles your mouth like a halo, you’re not imagining it. This is perioral dermatitis, and it’s more common than you think - especially in women between 16 and 45. The good news? It’s not contagious. The better news? You can get it under control. But only if you stop treating it like regular acne and start treating it like what it really is: an overreactive skin response to everyday products you probably think are harmless.
What’s Really Causing Your Rash?
Most people assume their skin flare-up is from stress, diet, or bad hygiene. But the real culprit? Often, it’s something you’re using every day without thinking. The #1 trigger for perioral dermatitis is topical steroids. Yes, even the little hydrocortisone cream you grabbed from the pharmacy for a bug bite or sunburn. If you’ve used it on your face for more than two weeks, you’re likely in the 85% of cases directly linked to steroid use. It starts with relief - the redness fades, the skin feels calmer. Then, when you stop, it comes back worse. That’s called rebound inflammation. And it traps you in a loop you didn’t even know you were in. But steroids aren’t the only offenders. Your moisturizer might be making things worse. Heavy creams with petroleum jelly, dimethicone, or beeswax? They create a barrier so thick your skin can’t breathe. That’s why 45% of cases are triggered by occlusive products. Even your sunscreen could be the problem. Physical sunscreens with zinc oxide or titanium dioxide above 10%? They’re meant to protect, but for sensitive skin, they can irritate. In fact, 22% of patients see flare-ups from these ingredients. Then there’s your toothpaste. Fluoride isn’t just for your teeth - it’s a trigger for 37% of people with perioral dermatitis. Sodium fluoride at 1,000-1,500 ppm is the usual suspect. You’re brushing twice a day, rinsing, but some residue lingers near your lips. That’s enough to keep the inflammation going. Switching to a non-fluoridated toothpaste with less than 0.1% sodium lauryl sulfate can lead to noticeable improvement in just 4 to 6 weeks. Hormones play a role too. For women, symptoms often worsen before their period - 72% report this pattern. Birth control pills contribute in about 28% of cases. And don’t overlook chewing gum or dental fillings - they’re less common, but still real triggers for 19% and 12% of patients respectively. Even environmental factors like wind and UV exposure make it worse. Sixty-three percent of people say sun exposure aggravates their rash.Why Your Current Skin Care Isn’t Working
You’re probably washing your face twice a day. Maybe using a foaming cleanser. Applying a thick moisturizer. Layering on sunscreen. Using foundation to cover the redness. Sounds normal, right? But here’s the problem: every one of those steps is likely making things worse. Foaming cleansers strip your skin’s natural barrier. That’s why 88% of people with perioral dermatitis see flare-ups from washing too often or with harsh products. Your skin isn’t oily - it’s damaged. So you don’t need a deep clean. You need a gentle reset. Moisturizers marketed as “hydrating” often contain ingredients that clog pores or trigger inflammation. Ceramides are good - but only in the right amount. Too much, and they become occlusive. Hyaluronic acid is great for hydration, but concentrations above 1% can draw moisture out of dry skin, making it feel tighter and more irritated. The sweet spot? 0.5-2% ceramides and under 1% hyaluronic acid. Sunscreen is tricky. Mineral sunscreens with high zinc or titanium dioxide? They’re often the culprit. Even “lightweight” versions can cause reactions. The fix? Look for liquid or gel formulas with mineral filters under 5%. Or better yet - protect your skin with a wide-brimmed hat. Physical barriers work better than chemical ones for this condition. And makeup? Skip the foundation. Even if it’s labeled “non-comedogenic,” many contain isopropyl myristate or other pore-clogging agents. If you must wear color, choose products with titanium dioxide below 3% and zero fragrance. Less is more - seriously. Three products max.The Gentle Skin Care Routine That Actually Works
Forget the 10-step routines. For perioral dermatitis, simplicity saves skin. Here’s what works based on real patient outcomes and clinical data:- Cleanse once a day, only with water or a non-foaming cleanser. Use a pH-balanced cleanser (5.5-6.5) like Cetaphil Gentle Skin Cleanser. No scrubbing. No hot water. Just pat dry with a soft towel.
- Moisturize with a minimal, ceramide-based cream. Vanicream Moisturizing Cream (0.5% ceramide) is a top pick among patients. Avoid anything with petrolatum, dimethicone, or fragrances.
- Use a light, low-mineral sunscreen. EltaMD UV Clear Broad-Spectrum SPF 46 (4.7% zinc oxide) is frequently cited in patient forums as a winner. Apply only if you’re going outside for more than 15 minutes.
When You Need More Than Skin Care
Sometimes, gentle care isn’t enough. If your rash is spreading, painful, or not improving after 4-6 weeks of a clean routine, you may need medical help. Topical metronidazole 0.75% gel works for 70% of patients after 8 weeks. It’s applied twice daily and has minimal side effects. Pimecrolimus 1% cream is another option - 65% improvement, no antibiotics involved. Both are prescription-only. For moderate to severe cases, oral antibiotics are used. But not the old-school 100mg doxycycline. That causes stomach issues in nearly half of users. The newer 40mg modified-release version? It clears 85% of cases with only 12% side effects. Treatment lasts 8-12 weeks. Don’t stop early - 40% of people relapse if they quit before the full course. Some patients benefit from dietary changes. If you have gluten sensitivity, going gluten-free helped 43% of cases in one clinical study. But for the general population? Only 12% see improvement. So don’t assume diet is the answer - but if you suspect a food trigger, try eliminating one thing at a time.What Doesn’t Work (And Why)
Here’s what you need to stop doing:- Using hydrocortisone cream on your face - even if it’s “over-the-counter” or “mild.”
- Applying coconut oil, olive oil, or tea tree oil - they’re natural, but they clog pores and irritate.
- Wearing heavy makeup - even “clean beauty” brands often contain trigger ingredients.
- Exfoliating with scrubs, AHAs, BHAs, or microdermabrasion - your skin barrier is already compromised.
- Switching products every week - consistency is key. Give each step at least 4 weeks to work.

Real Stories, Real Results
One woman in Melbourne stopped using her daily facial moisturizer and switched to Vanicream after 18 months of failed treatments. Within 3 weeks, the redness around her mouth began to fade. She’d been using hydrocortisone for years - thinking it was eczema. She didn’t know it was making it worse. Another patient switched from fluoride toothpaste to a sodium lauryl sulfate-free version. Within a month, her burning sensation disappeared. She’d been using the same toothpaste for 10 years. These aren’t outliers. They’re the norm. The Cleveland Clinic found that 85% of patients who followed a strict gentle skin care plan reported major quality-of-life improvements after 12 weeks. But 40% still felt anxious during the first few weeks - because the rash got worse before it got better.How to Prevent It From Coming Back
Once your skin clears, don’t go back to old habits. Recurrence rates are 40-60% if triggers aren’t permanently removed. Keep your routine simple. Stick to your three-step plan. Avoid steroid creams unless prescribed for a short, medical reason. Check ingredient labels like a detective. If you see dimethicone, petrolatum, or sodium fluoride - skip it. Carry a small list of safe products with you when shopping. Use apps that scan barcodes for irritants. Ask your pharmacist for non-fluoridated toothpaste options. And if you ever feel a flare-up coming back - go back to basics. Water. Minimal moisturizer. No makeup. No steroids. Perioral dermatitis doesn’t define you. But how you treat it? That does. This isn’t about perfection. It’s about patience. Your skin has been through a lot. Give it the quiet, gentle care it needs. And it will heal.Can perioral dermatitis go away on its own?
Sometimes, but rarely without changes to your routine. Most people see flare-ups return because the triggers - like steroid creams, heavy moisturizers, or fluoride toothpaste - are still being used. Without removing those, the condition tends to linger or come back worse. A gentle skin care routine and trigger avoidance are necessary for lasting improvement.
Is perioral dermatitis the same as acne?
No. Acne has blackheads and whiteheads (comedones), while perioral dermatitis doesn’t. The rash is usually made of tiny red bumps or pustules that circle the mouth, often sparing the lip border. It’s also more common in women aged 16-45 and is linked to topical steroids and skincare products, not oil production or clogged pores like acne.
How long does it take to clear up?
It varies. Most people see improvement after 2-4 weeks of stopping steroids and switching to gentle products. Full clearance usually takes 6-12 weeks. If you’re using prescription creams or oral antibiotics, you’ll need to complete the full course - even if your skin looks better sooner - to prevent recurrence.
Can I wear makeup with perioral dermatitis?
It’s best to avoid makeup until your skin clears. If you must wear it, choose fragrance-free, non-comedogenic products with titanium dioxide under 3%. Mineral powders are safer than liquid foundations. Always remove makeup gently with water only - no wipes or cleansers. Many patients find they don’t need makeup at all once the redness fades.
Why does my skin get worse before it gets better?
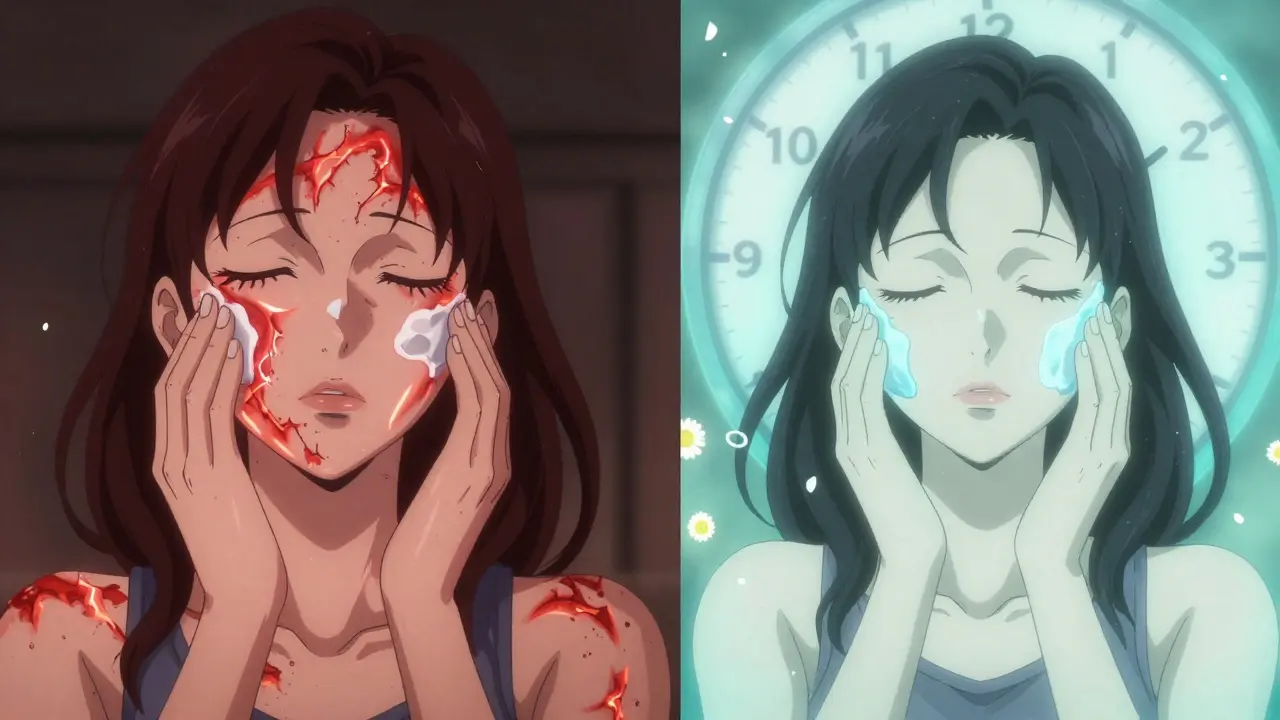
This is called a “steroid rebound” or withdrawal flare. If you’ve been using topical steroids - even for a short time - your skin becomes dependent. When you stop, your body reacts with increased inflammation. It’s not a sign the treatment isn’t working. It’s your skin adjusting. Most people see improvement after 7-14 days. Stick with the gentle routine - this phase usually passes.
Are natural remedies safe for perioral dermatitis?
Most aren’t. Coconut oil, tea tree oil, apple cider vinegar, and aloe vera may seem gentle, but they can clog pores, irritate sensitive skin, or trigger reactions. Even “natural” doesn’t mean safe for perioral dermatitis. Stick to clinically tested, minimal-ingredient products. Your skin needs stability, not experimentation.


Aayush Khandelwal
January 1 2026Yo, this post is basically the gospel of derm-adjacent enlightenment. I was using hydrocortisone like it was face mist for 14 months-thought I had ‘sensitive skin.’ Turns out I had steroid dependency masquerading as eczema. Switched to Vanicream, nixed fluoride toothpaste (yes, the minty one), and within 3 weeks the halo around my mouth? Gone. No magic. Just brutal simplicity. The 40mg doxycycline mod-release? Game-changer. My derm called it ‘the quiet revolution.’