Workplace Medication Safety Risk Calculator
Medication Risk Assessment
Hazardous Drug Exposure Assessment
Assessment Results
Please complete the assessment to see your risk level.
Every day, millions of workers take medications to manage pain, anxiety, or chronic illness. At the same time, others handle powerful drugs as part of their job-drugs that can harm them if they’re not handled right. These two realities collide in workplaces, creating hidden dangers that aren’t always visible until it’s too late. Whether you’re a nurse handling chemotherapy drugs, a factory worker on opioids for back pain, or a pharmacist mixing prescriptions, the risks are real-and they’re preventable.
Medications That Slow You Down at Work
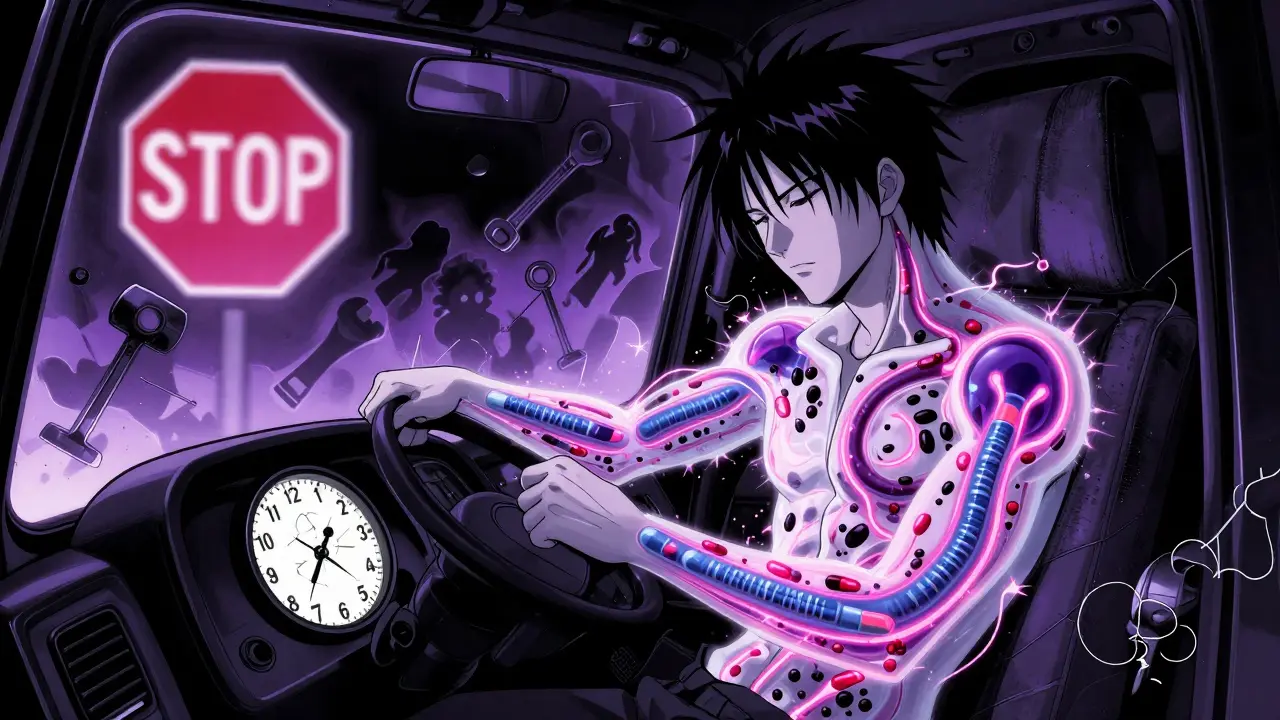
It’s not just about getting high. Prescription opioids and benzodiazepines are commonly prescribed for work-related injuries and stress, but they come with serious side effects that affect job performance. Opioids, taken by 18.7% of U.S. workers with musculoskeletal injuries, can cause drowsiness, slowed reaction time, and poor decision-making. Benzodiazepines, used by 7.2% of workers dealing with stress, can make you feel dizzy, confused, or uncoordinated. When taken together, the risk of a serious workplace accident jumps by 84%, according to a 2017 study in the Journal of Occupational and Environmental Medicine.
Think about it: a truck driver on oxycodone might miss a stop sign. A welder on alprazolam might lose grip on a tool. A machine operator with both drugs in their system? That’s a recipe for a catastrophic mistake. The CDC found that workers taking opioids are 2.1 times more likely to suffer a workplace injury than those who don’t. And it’s not just physical jobs. Office workers on these drugs are more prone to errors in data entry, missed deadlines, or miscommunication.
Some employers have drug-free workplace policies, and yes, they reduce incidents by 42%. But here’s the catch: 32% of workers who needed these medications for legitimate medical reasons lost their jobs-not because they were unsafe, but because the policy didn’t account for their condition. The real solution isn’t blanket bans. It’s better communication, individual risk assessments, and alternatives like physical therapy or non-opioid pain management.
Hazardous Drugs in the Workplace
Now flip the script. What if you’re not taking the drugs-you’re handling them? Healthcare workers, pharmacists, and lab technicians are exposed daily to antineoplastic drugs, chemotherapy agents, and other hazardous medications. These aren’t just strong drugs. They’re classified as carcinogenic, teratogenic, or toxic to organs-even at tiny doses.
The NIOSH 2024 List identifies 370 hazardous drugs. Of those, 267 are antineoplastic agents used to treat cancer. Even if you’re not the patient, you can still be harmed. Exposure happens through the air, skin contact, or contaminated surfaces. Inhalation accounts for 38% of exposures. Skin contact from splashes or dirty surfaces? That’s another 51%. And yes, even a tiny amount left on a counter or glove can get absorbed through your skin.
Workers exposed over time face real health consequences. A CDC meta-analysis of 47 studies found they have 2.3 times higher risk of miscarriage, birth defects, or infertility. Nurses and pharmacists who handle these drugs regularly report rashes, hair loss, nausea, and chronic fatigue. One chemotherapy nurse on Reddit described developing persistent skin rashes after three years on the job-even while following all safety protocols. Surface tests in her facility showed contamination in 68% of work areas.
How Exposure Happens (And How to Stop It)
Exposure isn’t random. It follows patterns:
- 38%: Inhalation of aerosols during drug preparation or administration
- 29%: Splashes to skin or eyes during IV bag changes
- 22%: Touching contaminated surfaces like counters, keyboards, or trash bins
- 7%: Accidental ingestion from poor hand hygiene
- 4%: Needlestick injuries
There are proven ways to cut these risks. Engineering controls are the most effective. Closed-system transfer devices (CSTDs) reduce surface contamination by 94.7%. These are special connectors that prevent drugs from escaping into the air during mixing or transfer. Facilities that installed them saw a drop from 42% to 4.7% contamination in just six months.
But equipment alone isn’t enough. Training matters. Workers need 16-24 hours of initial training, plus 4-8 hours every year. Many facilities skip this. A CDC field study found 43% of staff didn’t properly wear gloves, gowns, or masks. That’s not laziness-it’s often because training was rushed, unclear, or not reinforced.
And then there’s ventilation. One in three facilities have air handling systems that can’t capture vapors. One in four have cabinets that don’t seal right. These aren’t minor issues. They’re system failures.
Who’s Protected? Who’s Not?
Here’s the ugly truth: not everyone is covered. OSHA’s Hazard Communication Standard (29 CFR 1910.1200) only applies to about 6.2 million U.S. workplaces. That leaves 1.8 million healthcare workers in places like small clinics, home care agencies, or outpatient labs without federal protection. Meanwhile, the U.S. Pharmacopeia’s General Chapter 800 (USP 800) sets stronger standards-but it only applies to compounding pharmacies. That’s about 58,000 workers. The rest? Left to guesswork.
Unionized workers fare better. AFL-CIO data shows they experience 22% fewer medication-related incidents. Why? Because unions push for better training, safety equipment, and reporting systems. Non-unionized settings often lack those protections.
Large hospitals with 200+ beds are 2.3 times more likely to have full hazardous drug programs than small clinics. That means a nurse working at a rural outpatient center might be handling the same drugs as someone in a major cancer center-but with no safety cabinet, no CSTDs, and no regular monitoring.
What’s Changing in 2025?
Things are shifting. In February 2024, NIOSH removed liraglutide and pertuzumab from its hazardous drugs list after new data showed lower exposure risks. That’s progress. The FDA now requires boxed warnings on 27 antineoplastic drugs about occupational exposure risks. That’s the first time drug labels have included workplace safety info.
OSHA is expected to propose a Permissible Exposure Limit of 0.1 ng/cm² for hazardous drug surfaces by late 2024. That’s a tiny amount-equivalent to a grain of salt spread over a credit card. If enforced, it will force facilities to upgrade their controls.
Meanwhile, AI is stepping in. Johns Hopkins Hospital is testing a system that uses sensors and machine learning to predict high-risk moments during drug handling. In early trials, it predicted exposure events with 92% accuracy. Imagine a system that alerts you before you touch a contaminated surface-before you get sick.

What You Can Do
If you’re a worker:
- Know your drugs. If you’re on opioids or benzodiazepines, talk to your doctor about alternatives. Ask: “Could this affect my ability to do my job safely?”
- If you handle hazardous drugs, demand proper PPE, CSTDs, and ventilation. Don’t accept “we’ve always done it this way.”
- Report contamination. Even a faint smell or sticky surface could mean exposure.
- Join or support workplace safety committees. Your voice matters.
If you’re an employer:
- Don’t just rely on drug tests. Use risk assessments tailored to each role.
- Invest in CSTDs and ventilation upgrades. The return on investment? Lower injury rates, fewer workers’ comp claims, and better staff retention.
- Train like your life depends on it-because it does. Annual refreshers aren’t optional.
- Track surface contamination. Use wipe tests. Make results public. Transparency builds trust.
The economic cost of these risks? $4.7 billion a year in the U.S. alone. That’s $2.1 billion in medical bills, $1.8 billion in lost productivity, and $800 million in workers’ compensation. This isn’t just a health issue. It’s a financial one.
Final Thought
Medications save lives. But they can also endanger them-if we ignore how they interact with work. The answer isn’t to ban drugs. It’s to understand them. To respect them. To build systems that protect everyone: the worker on pain meds, the nurse mixing chemo, the pharmacist filling prescriptions. Safety isn’t a policy on a wall. It’s a habit. A culture. A commitment. And it starts with knowing the real risks-and doing something about them.
Can taking prescription opioids at work really increase injury risk?
Yes. Workers taking prescription opioids are 2.1 times more likely to suffer a workplace injury, according to CDC NIOSH data from 2018. Opioids can cause drowsiness, slowed reaction time, and impaired coordination-risks that are especially dangerous in jobs requiring precision, alertness, or heavy machinery. Even if you feel fine, your body may still be affected. The risk rises sharply if opioids are combined with benzodiazepines, increasing fall and accident risk by 84%.
Which healthcare workers are most at risk from hazardous drugs?
The highest-risk groups are nurses and pharmacists in oncology units, chemotherapy preparation areas, and compounding pharmacies. Ambulatory surgery centers and home health aides who administer drugs also face significant exposure. According to CDC data from 2023, 98% of hazardous drug exposures occur in healthcare settings-with pharmacies (32%), oncology units (28%), and surgery centers (19%) being the top three sources.
Are there legal protections for workers handling hazardous drugs?
Only some. OSHA’s Hazard Communication Standard applies to about 6.2 million U.S. workplaces, but leaves 1.8 million healthcare workers uncovered-especially those in small clinics or home care. The U.S. Pharmacopeia’s Chapter 800 provides stronger protections, but only applies to compounding pharmacies. Many workers rely on employer policies or union contracts for safety, which vary widely. There is currently no federal mandate covering all healthcare workers handling hazardous drugs.
How can employers reduce exposure to hazardous drugs?
The most effective methods are engineering controls: closed-system transfer devices (CSTDs) reduce contamination by 94.7%, according to WorkSafeBC. Proper ventilation, dedicated drug prep areas, and regular surface testing also help. Training is critical-workers need 16-24 hours of initial training and 4-8 hours annually. Facilities that combined CSTDs with behavioral training, like Mayo Clinic, reduced exposures by 89%. Administrative controls like no-eating policies and strict handwashing rules also cut risk.
What’s new in hazardous drug safety in 2024-2025?
In February 2024, NIOSH removed liraglutide and pertuzumab from its hazardous drugs list after new evidence showed lower exposure risk. The FDA now requires boxed warnings on 27 antineoplastic drugs about occupational hazards. OSHA is expected to propose a surface contamination limit of 0.1 ng/cm² by late 2024. AI monitoring systems are being piloted at hospitals like Johns Hopkins with 92% accuracy in predicting exposure events. These changes signal a shift toward science-based, proactive safety-not just reactive policies.


Tasha Lake
February 10 2026Okay, so let’s unpack this. Opioids + benzodiazepines are a perfect storm for workplace accidents-especially in high-stakes environments like ORs or ERs. The pharmacokinetics alone are terrifying: CYP3A4 inhibition, GABA potentiation, CNS depression synergy. And we’re not even talking about the metabolic lag-half-lives mean you’re still impaired 12 hours after your last dose. The CDC’s 2.1x injury multiplier? That’s conservative. I’ve seen NIOSH exposure logs where nurses on chronic opioids had 3.4x higher near-miss rates. We need individualized risk stratification, not blanket policies. CDTs aren’t just nice-to-haves-they’re biomechanical barriers against catastrophe.