When you pick up a prescription, you might see two options: the familiar brand name you’ve heard on TV, or a cheaper generic version with a plain label. Most people assume they’re the same. And for many drugs, they are. But when it comes to long-term safety, the story gets more complicated - especially for people taking medications every day for years.
Are generics really the same as brand-name drugs?
The FDA says yes. To get approved, a generic drug must contain the exact same active ingredient, strength, dosage form, and route of administration as the brand-name version. It must also prove bioequivalence - meaning it gets absorbed into your bloodstream at nearly the same rate and amount. The standard? The 90% confidence interval for absorption must fall between 80% and 125% of the brand. That sounds strict. And technically, it is. But here’s the catch: 125% is a 25% variation on the high end. For some drugs, even a 10% difference can matter.What happens when people take generics for years?
A massive 2020 study in Austria tracked over 1 million people on chronic medications for five years. They compared outcomes between those on brand-name antihypertensives and those on generics. The results surprised many. People on generics had fewer heart attacks, strokes, and deaths. The death rate for brand users was 53.8 per 1,000 patient-years. For generics? Just 30.2. That’s more than 40% lower. The same pattern held for major cardiac events. The researchers didn’t find a single case where the brand was safer. In fact, generics performed better - and the difference held up even after adjusting for age, income, and prior health conditions. But that’s not the whole picture.When switching to generics causes real problems
Case reports tell a different story. One patient switched from brand-name Ciproxin to a generic version of ciprofloxacin and kept getting infections. Symptoms didn’t clear until they switched back. Another patient on generic levofloxacin developed a persistent fever that vanished only after returning to the brand. These aren’t rare flukes. A 2013 review found that about 30% of patients who switch from brand to generic experience either no change, side effects, or worsening symptoms - enough to stop taking the drug entirely. Why does this happen? It’s not about the active ingredient. It’s about the rest of the pill.Inactive ingredients matter more than you think
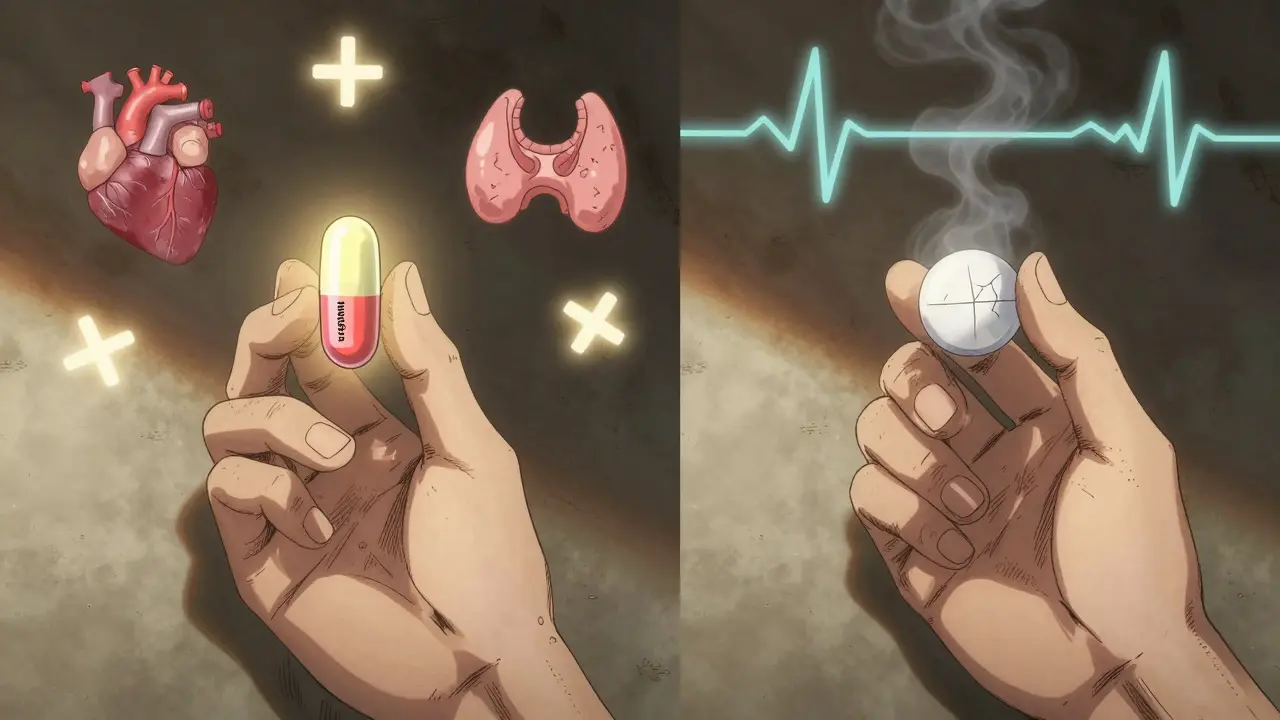
Generics don’t have to match the brand’s fillers, dyes, binders, or coatings. These inactive ingredients can affect how the drug dissolves in your stomach, how fast it’s absorbed, and even how your body reacts to it over time. For most people, this doesn’t matter. But for those with sensitive digestive systems, allergies, or conditions like epilepsy or thyroid disease, even tiny differences can trigger problems. Take levothyroxine, the most common thyroid medication. A 2017 study found that patients switching between generic brands had 12.3% more fluctuations in their TSH levels - the key marker for thyroid function - compared to those staying on Synthroid. That might sound small. But for someone with heart disease or an older adult, even a slight hormone shift can raise the risk of atrial fibrillation or bone loss.
Manufacturing location isn’t just a label - it’s a safety factor
Not all generics are made the same. A 2018 study from Ohio State University analyzed FDA adverse event data and found that generic drugs made in India were linked to 54% more severe adverse events - including hospitalizations and deaths - than those made in the U.S. This wasn’t true for every drug, but it held strong for older, widely used medications like ciprofloxacin. The Indian-made versions showed a 62% higher rate of serious side effects leading to hospital stays. Why? The study didn’t pinpoint one cause. But it’s likely a mix of inconsistent quality control, outdated facilities, and pressure to cut costs. The FDA inspects foreign plants, but they can’t be everywhere. And when a plant gets flagged for violations, it doesn’t mean the drugs are immediately pulled - they might still be on shelves for months.Authorized generics: the hidden middle ground
There’s another type of generic you might not know about: authorized generics. These are made by the original brand company, under a generic label, at the same factory. They’re chemically identical to the brand - down to the inactive ingredients. And here’s what the data shows: when researchers compared adverse event reports for amlodipine, the brand had 29.5% of reports, the authorized generic had 14.3%, and the regular generic had 56.2%. That’s a huge gap. But when they compared the authorized generic to the regular generic, the difference was minimal. That suggests most safety issues aren’t about brand vs generic - they’re about manufacturer.Who’s most at risk?
Not everyone needs to worry. For antibiotics, pain relievers, or antihistamines, switching to a generic is almost always safe. But for drugs with a narrow therapeutic index - where the difference between a helpful dose and a dangerous one is tiny - caution is critical. These include:- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin, carbamazepine (anti-seizure meds)
- Lithium (for bipolar disorder)
- Cyclosporine (organ transplant drug)
What does the big data say?
A 2021 Harvard study looked at over 136,000 seniors on three blood pressure drugs - losartan, valsartan, and candesartan. They compared ER visits and hospitalizations 12 months before and after generics hit the market. No increase in serious events. The results were statistically unchanged. But here’s the limitation: the study only tracked events that landed people in the hospital. It missed milder side effects - fatigue, dizziness, nausea - that might lead someone to stop taking the drug or lower their dose on their own. Meanwhile, the FDA’s own adverse event database shows 1,247 reports between 2018 and 2022 where people said the generic drug “didn’t work.” Only 289 reported the same for brand-name versions. But remember: generics make up 92% of all prescriptions in the U.S. So the raw numbers don’t tell the full story. The real question is: per prescription, which has a higher rate of failure?What should you do?
If you’re on a chronic medication - especially one with a narrow therapeutic index - don’t assume all generics are equal. Here’s what to do:- If you’re stable on a brand-name drug, don’t switch unless your doctor says it’s safe.
- If you’re switched to a generic and feel worse - fatigue, dizziness, worsening symptoms - don’t ignore it. Talk to your doctor. Ask if you can try the brand again.
- Ask your pharmacist if your generic is an authorized generic. If it is, it’s likely the safest option.
- For drugs like thyroid meds or seizure meds, stick with the same generic manufacturer if possible. Don’t let your pharmacy switch brands without telling you.
- Keep a symptom journal. Note changes in energy, mood, heart rate, or seizure frequency after any switch.
The bottom line
Generics save billions in healthcare costs. That’s a good thing. But safety isn’t just about whether the active ingredient matches. It’s about consistency, manufacturing quality, and how your body reacts over time. For most people, generics are safe and effective. But for a subset - especially those on critical, long-term meds - the difference between a brand and a generic can be life-changing. Don’t let cost savings override your health. If something feels off after a switch, speak up. Your body knows before your doctor does.Are generic drugs less safe than brand-name drugs?
For most medications, no - generics are just as safe. But for drugs with a narrow therapeutic index - like warfarin, levothyroxine, or anti-seizure meds - small differences in how the drug is absorbed can lead to serious side effects or treatment failure. Studies show some generics perform just as well or better than brands, but others - especially those made overseas - have higher rates of severe adverse events. Manufacturing quality and inactive ingredients matter more than most people realize.
Why do some people feel worse after switching to a generic?
It’s rarely the active ingredient. The issue usually lies in the fillers, coatings, or how the pill breaks down in your body. One person’s stomach might absorb a generic version slower than the brand, leading to lower drug levels. Others might react to a dye or binder in the generic that wasn’t in the brand. For people with sensitive systems - like those with thyroid disease or epilepsy - even tiny changes can trigger symptoms.
Should I avoid generics made in India or China?
Not all generics from those countries are unsafe, but studies show a clear pattern: drugs manufactured in India have been linked to significantly higher rates of severe adverse events - including hospitalizations and deaths - compared to U.S.-made versions. This is especially true for older, widely used drugs like ciprofloxacin. If you’re on a critical medication, ask your pharmacist where your generic is made. If you’re unsure, request the brand or an authorized generic.
What’s an authorized generic?
An authorized generic is made by the original brand-name company, under a generic label. It’s identical to the brand in every way - same factory, same ingredients, same quality control. It’s often cheaper than the brand but just as reliable. If your pharmacy offers it, it’s usually the safest generic option.
How do I know if my generic is causing problems?
Keep track of how you feel. If you start experiencing new side effects - fatigue, dizziness, mood changes, worsening symptoms - after switching to a generic, it might be the drug. Don’t assume it’s just your condition changing. Talk to your doctor. Ask if you can switch back to the brand temporarily. If symptoms improve, that’s a clue. Also, ask your pharmacist if your generic changed manufacturers - pharmacies sometimes switch without telling you.

Josh McEvoy
January 22 2026bro i switched my levothyroxine to generic and started feeling like a zombie 🥱 then my heart started doing the cha-cha… switched back to Synthroid and boom - energy returned. like, wtf is FDA thinking??