Thyroid Dose Adjustment Calculator
Current Levothyroxine Dose
Enter your current daily dose of levothyroxine (in micrograms)
TSH Increase
How much has your TSH increased since starting PPIs? (mIU/L)
PPI Type
Select which PPI you're taking
Enter your current dose and TSH increase to see your recommended adjustment.
Important: This calculator is based on clinical data showing typical adjustments. Always discuss dose changes with your doctor.
Why Your Thyroid Med Might Not Be Working
If you’re taking levothyroxine for hypothyroidism and also using a proton pump inhibitor (PPI) like omeprazole or pantoprazole for heartburn, your thyroid levels might be off-even if you’re taking both meds exactly as prescribed. This isn’t a myth or a guess. It’s a well-documented interaction that affects nearly 2.7 million Americans. The problem? PPIs reduce stomach acid, and levothyroxine needs that acid to be absorbed properly.
Levothyroxine is a synthetic version of the thyroid hormone T4. It’s the most common prescription in the U.S., with about 20 million people taking it every day. Most of them take generic tablets, which rely on stomach acid to dissolve and enter the bloodstream. That’s where PPIs come in. These drugs, used by over 15% of adults, shut down the acid-producing pumps in your stomach lining. That’s great for acid reflux-but terrible for levothyroxine absorption.
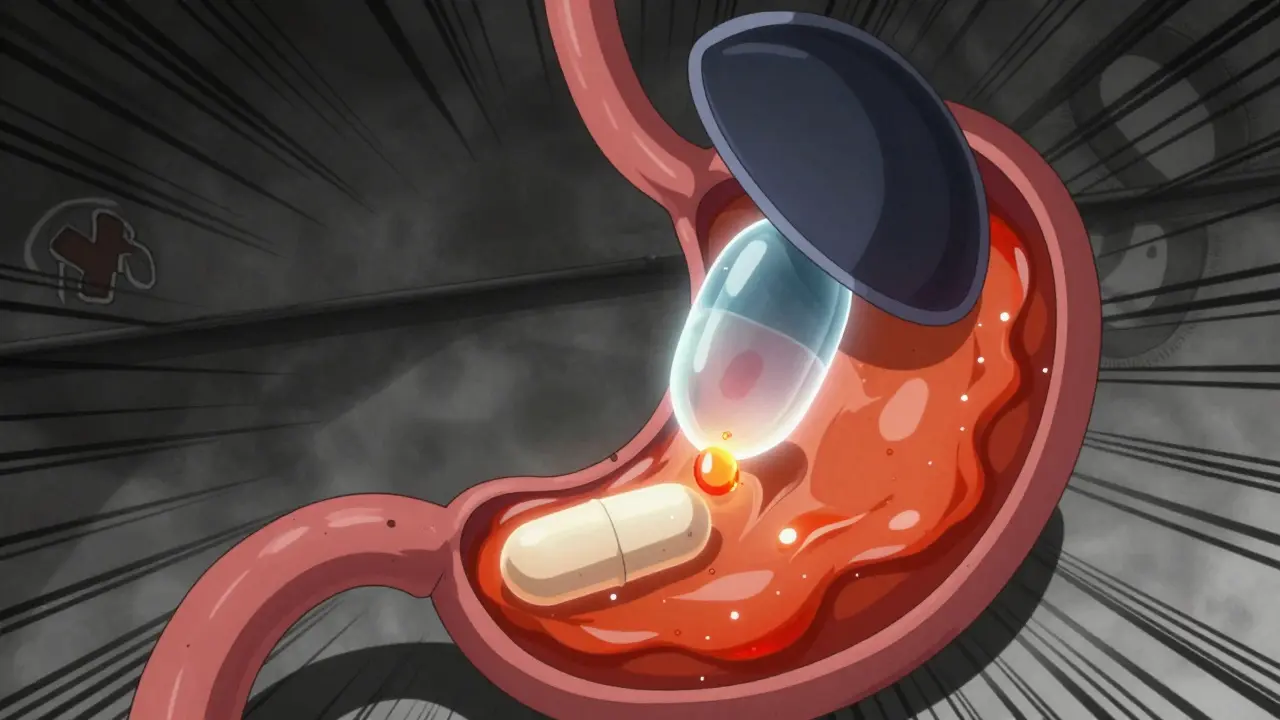
How PPIs Block Thyroid Hormone Absorption
Your stomach normally has a pH between 1 and 2-super acidic. That’s what breaks down levothyroxine tablets so your body can absorb them. PPIs raise that pH to 4 or higher. Think of it like trying to dissolve a sugar cube in water instead of vinegar. It just doesn’t work as well.
A 2021 review of seven clinical studies found that patients taking both drugs had consistently higher TSH levels, meaning their thyroid wasn’t getting enough hormone. In one study, even a standard 40mg daily dose of pantoprazole for just six weeks caused TSH to rise enough to require a levothyroxine dose increase. And it didn’t matter if they took the PPI in the morning with levothyroxine or at night-because PPIs don’t just work for a few hours. Their effect lasts up to 72 hours.
What the Numbers Show
According to data from the Mayo Clinic and the American Thyroid Association, 15-20% of people on both medications need their levothyroxine dose adjusted. The average increase? Between 12.5 and 25 micrograms per day. That’s not a tiny tweak-it’s enough to shift your whole hormone balance.
One study tracked patients who were stable on levothyroxine, then added a PPI. Within eight weeks, over 40% needed a higher dose. Another analysis of Reddit posts from 147 users showed that 68% reported needing more levothyroxine after starting PPIs. Common complaints? Fatigue (72%), weight gain (58%), brain fog, and cold intolerance-all classic signs of under-treated hypothyroidism.
Timing Doesn’t Fix It
You might have heard that taking levothyroxine and PPIs at different times of day can solve the problem. Some doctors still suggest waiting 4 hours between doses. But the science says otherwise.
A 2023 crossover study tested this exact idea. One group took levothyroxine at 6 a.m. and pantoprazole at 6 p.m. Another group did the opposite. Both groups saw the same rise in TSH. Why? Because PPIs don’t just turn off acid for a few hours-they keep the stomach neutral for days. Even if you take your thyroid med in the morning and your PPI at night, your stomach is still too alkaline by the time the levothyroxine needs to dissolve.
What to Do Instead
There are three real solutions-not just one.
- Switch to liquid levothyroxine: Tirosint-SOL is a gel capsule filled with levothyroxine dissolved in glycerin. It doesn’t need stomach acid to absorb. A 2019 study confirmed it works just as well whether taken with or without PPIs. The catch? It costs $350 a month, compared to $15-25 for generic tablets. Insurance doesn’t always cover it, but some patients say the energy boost and weight loss make it worth it.
- Try an H2 blocker instead: Famotidine (Pepcid) reduces acid too, but not as deeply or as long as PPIs. A 2018 study showed no significant change in TSH when famotidine was taken with levothyroxine. If you only need occasional heartburn relief, this might be a better fit. But if you’re on PPIs for chronic GERD, H2 blockers may not cut it.
- Reevaluate if you even need the PPI: Many people stay on PPIs for years-even when they don’t need them. A 2022 study found that 70% of long-term users could safely stop with a gradual taper. Ask your doctor: Is this still necessary? Could lifestyle changes (less caffeine, smaller meals, no late-night eating) help?
When to Test Your TSH
If you’re on both meds, don’t wait for symptoms to get worse. Get your TSH checked before you start the PPI, then again at 6-8 weeks. That’s the window when absorption changes show up in blood tests. After that, monitor every 3-6 months if you’re stable.
Doctors at the American Association of Clinical Endocrinologists recommend increasing levothyroxine by 12.5-25 mcg if TSH rises above the target range. Most patients stabilize within 12 weeks. But if you don’t test, you won’t know if your dose is still right.

What’s Coming Next
Researchers are working on new versions of levothyroxine that bypass the stomach entirely. Enteric-coated tablets are in phase 3 trials-these are designed to dissolve in the small intestine, not the stomach. If approved, they could eliminate this interaction entirely.
Meanwhile, the FDA is updating labeling rules to require clearer warnings on PPI and thyroid med packaging. And with Tirosint-SOL’s patent expiring in 2025, cheaper generic versions could become available, making this solution more accessible.
Real Talk: What Patients Are Saying
On Reddit’s r/Hypothyroidism subreddit, people share stories that go beyond numbers. One woman said she was exhausted for months until her doctor switched her to Tirosint-SOL. “I slept through the night for the first time in two years,” she wrote. Another man switched from omeprazole to famotidine and lost 15 pounds in three months without changing his diet.
But not everyone has options. Some can’t afford the liquid form. Others can’t stop their PPI without worsening reflux. That’s why personalized care matters. There’s no one-size-fits-all fix. But there are real, science-backed ways to manage this.
Bottom Line
If you’re taking levothyroxine and a PPI, your thyroid levels are probably not where they should be. This isn’t your fault. It’s a known, common, and often overlooked interaction. Don’t just keep taking both meds and hope for the best. Talk to your doctor. Get your TSH checked. Ask about alternatives. You deserve to feel like yourself again.

Eliana Botelho
January 29 2026Okay but have you ever considered that maybe your thyroid isn't the problem at all? Like, what if your gut is just totally wrecked from years of junk food and stress? I went on PPIs for three years and my TSH was fine, but my cortisol was through the roof. I stopped the PPI, started doing breathwork, and my energy came back. Nobody talks about the mind-body link. You can't just fix everything with pills. Your body's not a vending machine.