Every year, thousands of people walk into a pharmacy to pick up their medication-only to get someone else’s pills. It sounds impossible, but it happens more often than you think. A wrong-patient error occurs when a pharmacist or technician hands a prescription to the wrong person. The consequences can be deadly: someone with a peanut allergy gets an allergic reaction because they received a drug meant for another patient. Someone with high blood pressure misses their dose because they got a painkiller instead. These aren’t hypothetical risks-they’re real, preventable, and happening right now in pharmacies across the country.
Why Wrong-Patient Errors Are So Dangerous
Wrong-patient errors aren’t just mistakes. They’re safety failures with serious outcomes. According to the Institute for Safe Medication Practices (ISMP), these errors rank among the most dangerous types of medication mistakes. Why? Because they bypass every other safety check. Even if the drug is correct, the wrong person taking it can lead to harm. A diabetic might get insulin meant for someone else, causing a life-threatening drop in blood sugar. A child might get a high-dose opioid meant for an adult. Or worse-someone might not get their heart medication at all because it was given to the wrong person. The Joint Commission has tracked these errors since 2003. In 2023, medication-related wrong-patient incidents were still in the top five causes of sentinel events-serious, unexpected incidents that result in death or serious harm. And it’s not just hospitals. Community pharmacies are just as vulnerable. A 2022 report from the Agency for Healthcare Research and Quality found that medication errors send about 1.3 million people to U.S. emergency rooms each year. A significant portion of those are wrong-patient errors.The Two-Step Verification System That Works
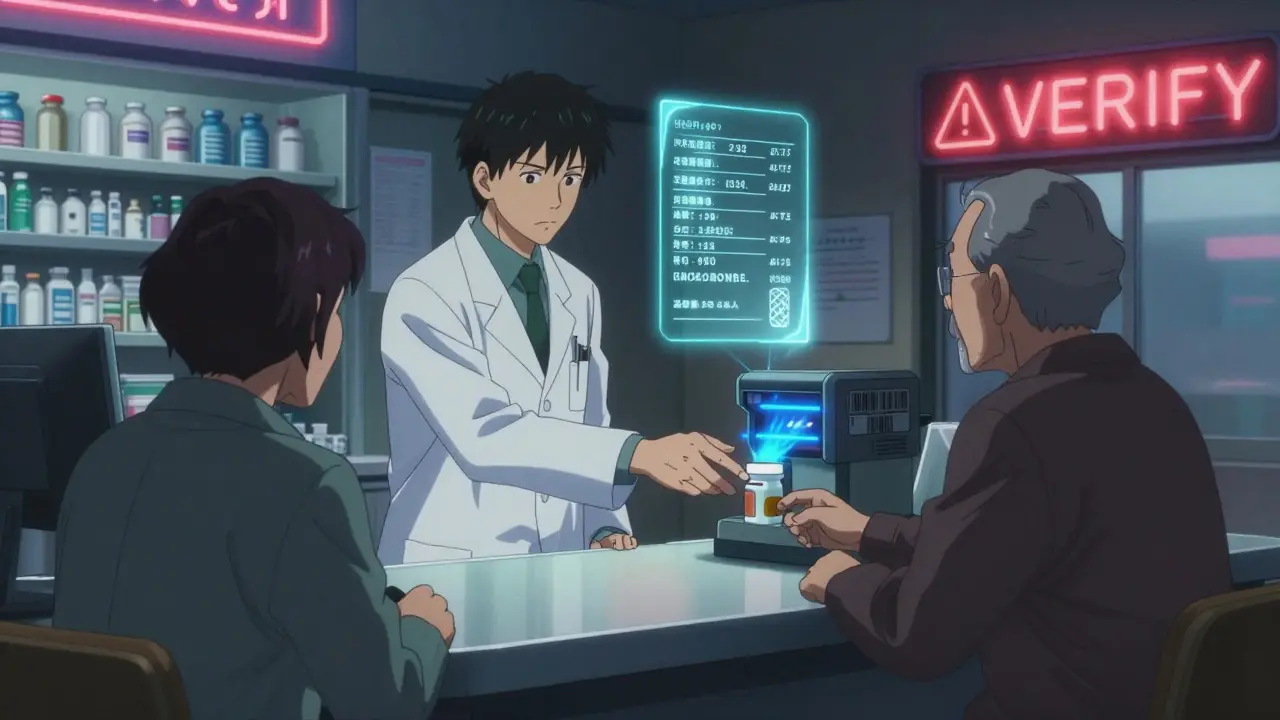
The simplest and most effective way to stop these errors is to verify the patient’s identity using two pieces of information before handing over any prescription. That means asking for the patient’s full name and date of birth-every single time. This isn’t just a suggestion. It’s now a standard practice in nearly all major pharmacy chains. CVS, Walgreens, and Walmart have required this since 2015-2018. The process is straightforward:- Ask the person picking up the prescription: “What’s your full name and date of birth?”
- Compare what they say to the name and DOB on the prescription label and in the pharmacy’s computer system.
- If anything doesn’t match-stop. Don’t dispense. Double-check.
Technology That Stops Errors Before They Happen
Manual checks help-but technology makes them foolproof. Barcode scanning systems are now common in chain pharmacies. Here’s how they work:- The patient scans a barcode on their ID card, phone app, or pharmacy loyalty card.
- The system matches the barcode to the prescription record.
- If the names don’t match, the system won’t allow the transaction to complete.
Why Counseling Is Your Last Line of Defense
The final safety net isn’t a machine-it’s a conversation. When the pharmacist hands the medication to the patient, they should take 30 seconds to confirm: “This is your blood pressure pill, right? You take it once a day, in the morning?” This isn’t just good customer service. It’s a critical safety step. Pharmacy Times reports that 83% of dispensing errors are caught during this final counseling moment. A patient might say, “Wait, I don’t take this,” or “I don’t have high blood pressure,” and that’s your chance to stop the error before it leaves the counter. Even if the patient doesn’t speak up, asking the question creates a moment of awareness. It gives the patient a chance to question what they’re getting. That’s powerful.
What Happens When You Combine All These Steps?
The most effective pharmacies don’t rely on just one method. They layer them. A 2023 study in the Journal of the American Pharmacists Association found that pharmacies using both dual-identifier verification and barcode scanning and patient counseling reduced wrong-patient errors by 89%. That’s almost elimination. Compare that to pharmacies using only name and DOB-those still saw 45% fewer errors, but errors still happened. The difference? Layered systems catch what humans miss. A tired tech might mishear a name. A barcode scanner doesn’t.Challenges and How to Overcome Them
No system is perfect. Staff report pressure during busy hours. Patients get annoyed being asked the same questions every time. Elderly patients sometimes forget their birthdate. Some think it’s “rude” or “suspicious.” Here’s how top-performing pharmacies handle it:- Train staff to explain why it matters. Instead of saying, “I need your DOB,” say, “This helps us make sure you get the right medicine. It’s happened before, and we don’t want that to happen to you.”
- Use signage. Post signs near the pickup counter: “We verify your identity to keep you safe.”
- Schedule wisely. Have extra staff on hand during peak times (lunch, after work) to avoid rushing.
- Record near-misses. If someone almost got the wrong med, log it. Not to punish, but to improve.
The Bigger Picture: Regulation and Costs
It’s not just about safety-it’s about money. A single wrong-patient error can cost an independent pharmacy $12,500 in legal fees, fines, and lost trust, according to the National Community Pharmacists Association. Medicare Part D plans now penalize pharmacies with error rates above 0.5%. That’s pushing even small shops to upgrade. The market for pharmacy safety tech is growing fast-from $1.2 billion in 2024 to $2.7 billion by 2028. But adoption isn’t equal. Hospital pharmacies? 89% use barcode scanning. Chain pharmacies? 76%. Independent pharmacies? Only 42%. Cost is the biggest barrier. Still, the cost of doing nothing is higher.
What’s Next? Biometrics and AI
Some pharmacies are testing even smarter tools. Walgreens launched a fingerprint verification pilot in 500 locations in January 2025. Early results show 92% accuracy. But privacy concerns are slowing rollout. Experts predict AI-powered facial recognition and voice matching will be standard in 70% of pharmacies by 2027. Imagine walking up, looking at a camera, and the system instantly confirms your identity-no card, no ID, no questions. But even the best tech won’t replace human judgment. As Dr. Michael Cohen of ISMP says: “Relying on vigilance alone is not enough. You need systems that make errors impossible.”What You Can Do as a Patient
You’re not just a recipient-you’re part of the safety team.- Always carry your ID or pharmacy card.
- Know your birthdate. If you’re helping an elderly parent, have it written down.
- Ask questions. “Is this the right medicine for me?”
- If you get a pill you don’t recognize, say so. Don’t assume it’s a new dosage.
What are the most common causes of wrong-patient errors in pharmacies?
The most common causes are similar-sounding patient names (like “John Smith” vs. “Jon Smith”), staff rushing during busy hours, failure to verify two patient identifiers, and patients picking up prescriptions for others without proper identification. Sound-alike names account for about 22% of these errors, according to ECRI Institute.
Is it mandatory for pharmacies to verify patient identity before dispensing?
Yes. As of 2024, the National Association of Boards of Pharmacy (NABP) updated its Model State Pharmacy Act to require dual-identifier verification (name and date of birth) for all prescription dispensing. While enforcement varies by state, major pharmacy chains and many independent pharmacies follow this standard to avoid liability and meet insurance requirements.
Can barcode scanning completely eliminate wrong-patient errors?
No system is 100% foolproof, but barcode scanning reduces wrong-patient errors by 63-78% when properly implemented. It works best when combined with staff verification and patient counseling. Errors can still occur if a barcode is scanned incorrectly, if the wrong patient’s card is used, or if the system isn’t updated with the latest prescription data.
Why do some patients get frustrated with repeated identification questions?
Many patients, especially older adults or those who visit the pharmacy frequently, feel like they’re being treated like a suspect. They don’t understand why they’re being asked the same thing every time. The key is education: staff who explain that this prevents deadly mistakes often turn frustration into appreciation. A 2024 ECRI survey found that 68% of patients feel safer when asked for ID.
What should I do if I think I received the wrong medication?
Don’t take it. Go back to the pharmacy immediately. Ask to speak with the pharmacist. Show them the prescription label and the medication you received. Most pharmacies have a safety protocol to investigate and replace the medication. If you’ve already taken it and feel unwell, call your doctor or go to the emergency room right away.
Are independent pharmacies less safe than chain pharmacies?
Not necessarily-but they often have fewer resources. Chain pharmacies are more likely to have barcode systems and automated verification software. Independent pharmacies may rely more on manual checks, which are effective if done consistently. The key isn’t the size-it’s whether the pharmacy has a strong safety culture, trained staff, and clear protocols. Many independent pharmacies have zero wrong-patient errors by prioritizing verification and patient communication.

steve rumsford
January 7 2026Man i’ve had my meds handed to me three times by mistake and never said anything cause i thought it was my new script. then i took it and felt like i got hit by a bus. never again.