Why Weight-Based Checks Are the Lifeline for Pediatric Medication Safety
Children aren’t just small adults. That simple truth is why pediatric medication errors happen so often - and why they’re so dangerous. A child’s dose isn’t just a smaller version of an adult’s; it’s calculated down to the milligram based on their exact weight. One wrong decimal point, one outdated weight entry, one missed conversion from pounds to kilograms - and you could be giving a child a toxic dose. The data doesn’t lie: children are three times more likely to suffer a medication error than adults. Most of these errors come down to weight-based miscalculations.
Think about it: a 12-pound infant needs a different dose than a 60-pound toddler. But in busy clinics, emergency rooms, or even community pharmacies, weights are often estimated, outdated, or entered in the wrong unit. A 2021 review of 63 studies found that over 32% of pediatric dispensing errors involved weight-based dosing mistakes. And 8.4% of those caused real harm - vomiting, seizures, organ damage. These aren’t rare accidents. They’re preventable failures.
The Three Critical Points Where Weight Checks Must Happen
Preventing these errors isn’t about one magic fix. It’s about building layers of protection - like seatbelts, airbags, and crash zones in a car. The Institute for Safe Medication Practices says the most effective approach is mandatory weight verification at three key moments: when the doctor writes the order, when the pharmacist fills it, and when the nurse gives it to the child.
At the prescribing stage, electronic health records (EHRs) should block any dose entry unless the patient’s current weight is entered. No weight? No prescription. Simple. Systems like Epic’s new Pediatric Safety Module 4.0 now use growth charts to flag doses that don’t match expected weight ranges. If a 5-year-old is prescribed a dose meant for a 100-pound teen, the system should scream. Not whisper. Scream.
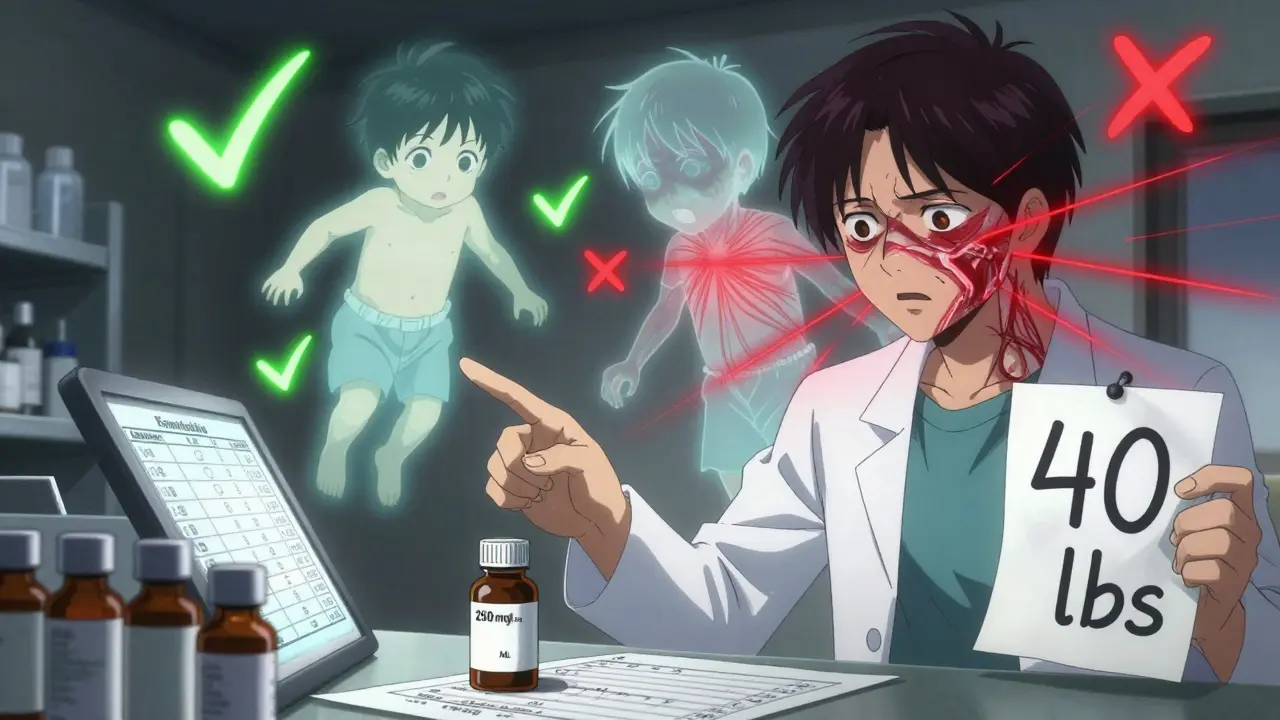
At the pharmacy, every pediatric prescription needs a second pair of eyes. Pharmacists must manually verify the weight-to-dose calculation - even if the computer did it. Why? Because computers make mistakes too. A 2021 study found that 41.7% of weight-based alerts were overridden by clinicians, and nearly 1 in 5 of those overrides were actual errors. That’s not alert fatigue - that’s a system failure. Pharmacies need a checklist: weight entered? In kilograms? Correct unit? Dose within safe range? Double-checked by a second pharmacist?
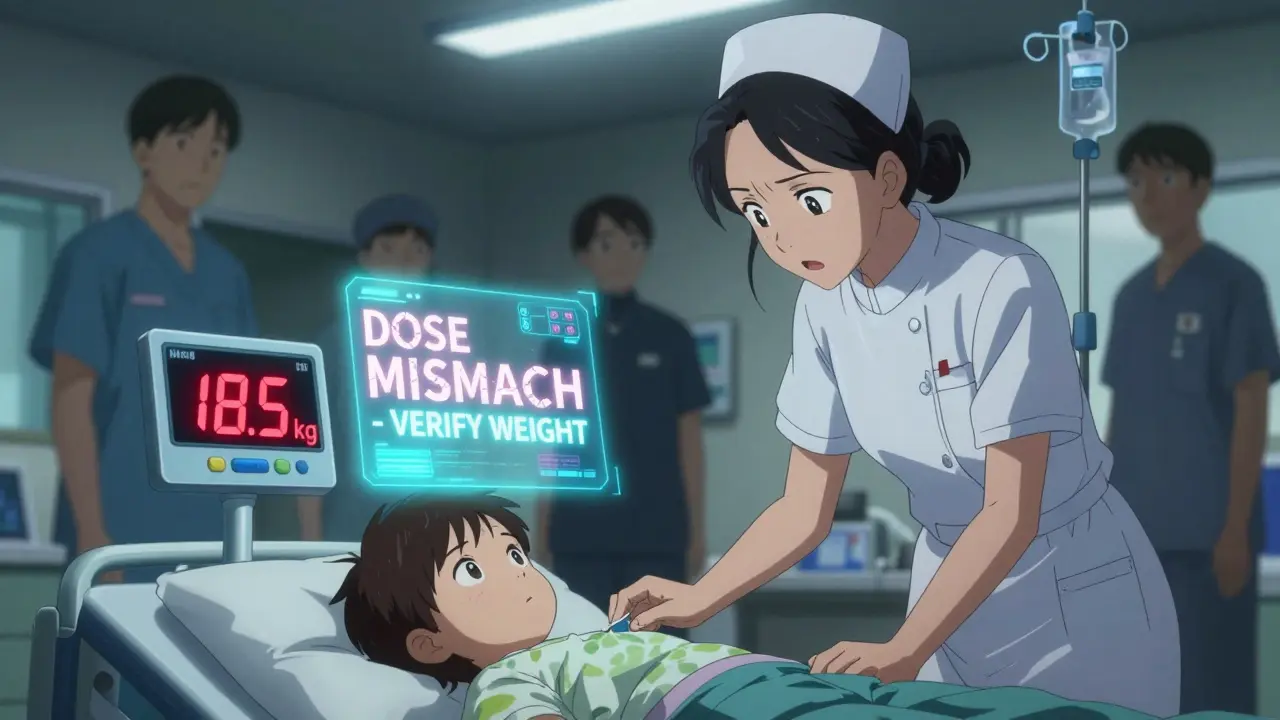
At the bedside, barcode scanning should link the child’s weight to the medication label. If the system knows the child weighs 18.5 kg and the vial says 20 mg/kg, but the dose is 450 mg instead of 370 mg, it should stop the nurse before the IV goes in. Studies show this step cuts administration errors by over 74%.
Why Kilograms Only - and No Exceptions
Here’s the most overlooked detail: all weights must be entered in kilograms only. No pounds. No stones. No guesses. The American Society of Health-System Pharmacists made this a hard rule in 2018 - and for good reason. Over 12% of pediatric dosing errors come from simple pound-to-kilogram conversions. A nurse hears "25 pounds" and multiplies by 0.45 - but if they use 0.4 instead, they’re off by 10%. That’s the difference between a safe dose and a dangerous one.
Real-world fix: Digital scales in pediatric units should display only kilograms, with precision to 0.1 kg for babies and 0.5 kg for older kids. No toggle button. No option to switch units. Just kg. Period. Boston Children’s Hospital saw weight conversion errors drop from 14.3 per 10,000 doses to just 0.8 after enforcing this rule. That’s a 94% reduction - all from removing one confusing step.
Community pharmacies struggle with this. Without direct EHR access, pharmacists often rely on caregivers to report weights. And caregivers? They think in pounds. They say, "My son’s 40 pounds." The pharmacist has to convert. And that’s where errors creep in. The solution? Ask for the weight in kilograms. If they don’t know it, weigh them on the spot. Keep a pediatric scale in the consultation room. It’s not extra work - it’s the difference between life and death.
Standardized Concentrations: The Silent Hero
Another hidden source of error? Variable drug concentrations. Imagine two different bottles of amoxicillin: one is 125 mg per 5 mL, another is 250 mg per 5 mL. A nurse grabs the wrong one, gives the same volume - and the child gets double the dose. This happens more than you think.
Facilities that standardize concentrations across all pediatric medications reduce calculation errors by over 72%. That means every child gets amoxicillin at the same strength - say, 250 mg/5 mL - no matter where they’re prescribed. It’s not about cost or availability. It’s about reducing cognitive load. When every dose calculation follows the same pattern, mistakes drop.
Some hospitals even use preprinted order sheets with dosing charts based on weight. In community settings, these can be lifesavers. But in big hospitals with complex cases, they’re not enough. That’s why standardization works best when paired with digital systems. The goal isn’t to replace technology - it’s to make it simpler.
What Happens When Systems Fail - And How to Fix Them
Technology isn’t perfect. Even the best EHRs flood staff with alerts. A 2022 study found that in some systems, pharmacists get 15-20 weight-based alerts per shift. Most are false alarms - like when a teenager nears adult weight and the system flags a normal adult dose as "too high." That’s alert fatigue. And when alerts become background noise, real dangers slip through.
So how do you fix it? First, tune the alerts. Don’t just use fixed weight thresholds. Use growth percentiles. Epic’s new module does this - it knows that a 14-year-old weighing 110 pounds isn’t a 5-year-old. Second, don’t rely on alerts alone. Train staff to question every dose that feels "off," even if the system says it’s fine. Third, make it easy to report near-misses without fear. The best safety cultures don’t punish mistakes - they learn from them.
And don’t forget the human factor. A 2022 survey found that 63% of pediatric nurses had seen weight documentation errors in the past year. Often, it’s because a child was weighed weeks ago and no one updated it. The fix? Mandatory weight checks within 24 hours for inpatients, and every 30 days for outpatients. If a child hasn’t been weighed in over a month, the system should flag the order and require a new measurement before dispensing.

Who’s Responsible - And What It Really Takes to Make This Work
This isn’t just the pharmacist’s job. Or the nurse’s. Or the doctor’s. It’s everyone’s. But someone has to lead it. That’s usually the pharmacy department. Successful programs assign 1.5 full-time pharmacists per 50 pediatric beds just for verification. That sounds expensive. But consider this: one preventable error can cost a hospital over $500,000 in lawsuits, fines, and lost trust.
Training is non-negotiable. Staff need 40 hours of education on pediatric pharmacokinetics - not a 10-minute PowerPoint. They need to understand how a child’s liver and kidneys process drugs differently than an adult’s. They need to know why a 10 mg/kg dose might be safe for a 6-month-old but deadly for a 2-month-old.
And here’s the hard truth: rural hospitals are falling behind. Only 33% have full weight-based systems, compared to 94% of children’s hospitals. That’s not fair. That’s not safe. If you work in a small clinic or community pharmacy, start small. Get a digital scale. Use a printed dosing chart. Make weight entry mandatory before any pediatric script is filled. You don’t need a $2 million EHR upgrade to save a life.
The Future Is Smarter - But Not Just Tech
The future of pediatric safety isn’t just about better software. It’s about smarter systems. The FDA is pushing for EHRs to integrate growth charts automatically. AI tools are being tested to predict a child’s expected weight based on age and past records - catching errors before they happen. Wearables might one day track weight changes in kids with chronic illnesses. Blockchain could lock weight data so it can’t be altered.
But here’s what no algorithm can replace: a human who asks, "Did we check the weight?" A nurse who says, "That dose feels high. Let me double-check." A pharmacist who takes five extra seconds to verify, even when the system says it’s fine.
Technology reduces errors. Culture prevents them. The most effective systems combine both - and never let convenience override caution. Because in pediatric care, there’s no room for "good enough."
Why is weight so critical in pediatric dosing?
Children’s bodies process medications differently than adults. Their liver, kidneys, and body fat percentages change rapidly with age and growth. Doses are calculated per kilogram of body weight - so even a small error in weight can lead to a dangerous overdose or underdose. A 10% weight error can mean a 10% dose error - which in a child can be life-threatening.
Can I just use pounds instead of kilograms?
No. Converting pounds to kilograms is a leading cause of pediatric dosing errors. The American Society of Health-System Pharmacists and the American Academy of Pediatrics require all weights to be documented and entered in kilograms only. Digital scales in pediatric settings should display only kilograms to eliminate conversion mistakes.
How often should a child’s weight be checked before giving medication?
For hospitalized children, weight must be measured within 24 hours of admission or before any new medication is given. For outpatient settings, weight should be verified every 30 days. If a child hasn’t been weighed in over a month, the prescription should be flagged and a new measurement required before dispensing.
What’s the biggest mistake pharmacists make with pediatric weights?
Relying on outdated or estimated weights. Many pharmacists assume a child’s weight hasn’t changed since their last visit - but kids grow fast. A child who weighed 15 kg six months ago might now weigh 18 kg. Giving the same dose can lead to a 20% overdose. Always verify current weight - don’t assume.
Do electronic health records really prevent these errors?
Yes - but only if they’re set up correctly. Studies show EHRs with integrated clinical decision support reduce pediatric dosing errors by up to 87%. But if alerts are too frequent or poorly tuned, staff start ignoring them. The key is configuring alerts to match your facility’s patient population and using growth percentiles, not fixed weight limits.
What should I do if I suspect a weight-based dosing error?
Stop. Don’t give the medication. Verify the weight. Recalculate the dose. Consult a pharmacist or senior clinician. Report the near-miss - even if no harm occurred. Most systems have anonymous reporting tools. These reports help improve safety protocols for everyone.

Naresh L
February 2 2026It’s funny how we treat kids like miniature adults in medicine-until something goes wrong, then suddenly we remember they’re not just small humans. Weight isn’t just a number; it’s a lifeline. I wonder how many of these errors happen because we’re too busy optimizing for efficiency instead of safety. The system rewards speed, not scrutiny. And yet, one decimal point can end a life. Maybe the real problem isn’t the tech-it’s the culture that lets us ignore it.