When your doctor orders pulmonary function tests, it’s not just another checkbox. These tests-especially spirometry and DLCO-can reveal what’s really going on inside your lungs, even when you feel fine. Many people assume normal breathing means healthy lungs. But that’s not always true. You could have early lung damage and still take a full breath without trouble. That’s why these tests matter.
What Spirometry Actually Measures
Spirometry is the most common lung test you’ll ever take. You breathe in as deep as you can, then blow out as hard and fast as you can into a tube connected to a machine. It sounds simple. But the numbers it produces tell a detailed story.
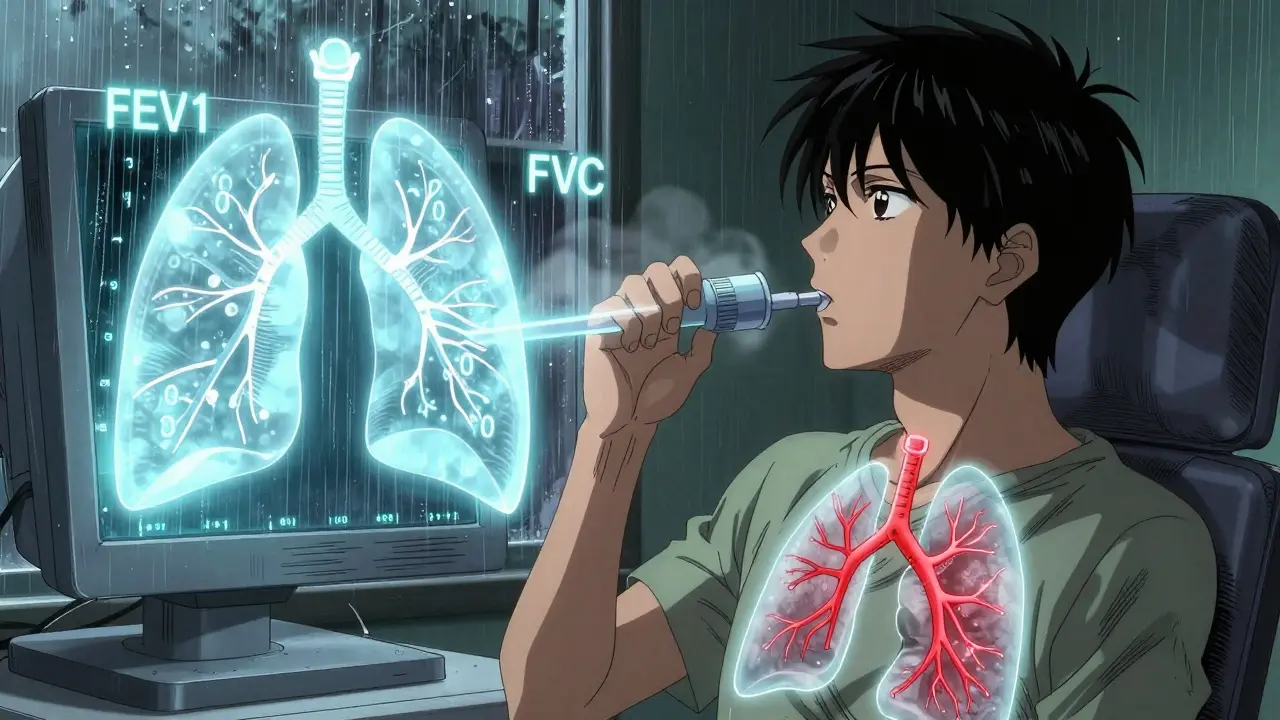
The two most important numbers are FEV1 and FVC. FEV1 is how much air you can force out in the first second. FVC is the total amount you can blow out in one full breath. The ratio between them-FEV1/FVC-is the real key.
If your FEV1/FVC ratio is below 0.7, you likely have airflow obstruction. That’s the hallmark of asthma, COPD, or chronic bronchitis. Your airways are narrowed, so it takes longer to empty your lungs. You might not feel it yet, especially if you’re young or active. But the machine sees it.
If both FEV1 and FVC are low but the ratio is normal or even high, that’s restriction. Your lungs aren’t expanding fully. This could be from scarring (like pulmonary fibrosis), obesity, or a curved spine. But here’s the catch: spirometry alone can’t tell you why your lungs aren’t expanding. That’s where DLCO comes in.
Why DLCO Is the Hidden Key
DLCO stands for diffusing capacity of the lung for carbon monoxide. It doesn’t measure airflow. It measures how well oxygen moves from your lungs into your blood. That’s a big deal. Many lung diseases don’t block airways-they damage the tiny air sacs (alveoli) or the blood vessels around them.
The test is more complex. You inhale a tiny, safe amount of carbon monoxide mixed with helium and oxygen. You hold your breath for exactly 10 seconds-no more, no less-then exhale. The machine measures how much CO was absorbed. That tells you how efficiently your lungs transfer gas.
Normal DLCO is between 75% and 140% of what’s predicted for your age, height, and sex. Below 75%? That’s a red flag. Above 140%? That’s unusual but can happen in some conditions too.
Here’s what’s critical: DLCO can be low even when spirometry looks perfect. That’s how you catch early emphysema or interstitial lung disease before you’re coughing or wheezing. In fact, DLCO drops in early fibrosis 12 to 18 months before spirometry changes. That’s a huge window for early treatment.
Putting It Together: The Real Diagnostic Patterns
Doctors don’t look at these tests in isolation. They combine them. Here’s what the patterns mean in real life:
- Low FEV1/FVC + Normal DLCO → Classic asthma or COPD. Airway narrowing, but gas exchange is still okay.
- Low FVC + Low DLCO → Likely interstitial lung disease (like pulmonary fibrosis). The lung tissue is scarred, so both volume and gas transfer suffer.
- Low FVC + Normal DLCO → Probably not a lung problem. Could be obesity, weak muscles, or a curved spine. Your lungs work fine-you just can’t expand them fully.
- Normal spirometry + Low DLCO → This is where people get missed. Could be early emphysema, pulmonary hypertension, or even small blood clots in the lungs (chronic pulmonary emboli). You might feel short of breath climbing stairs, but your doctor thinks you’re just out of shape. DLCO catches this.
- High DLCO → Less common, but can happen in asthma during flare-ups, severe anemia, or heart shunts. It’s not always a bad sign-but it needs context.
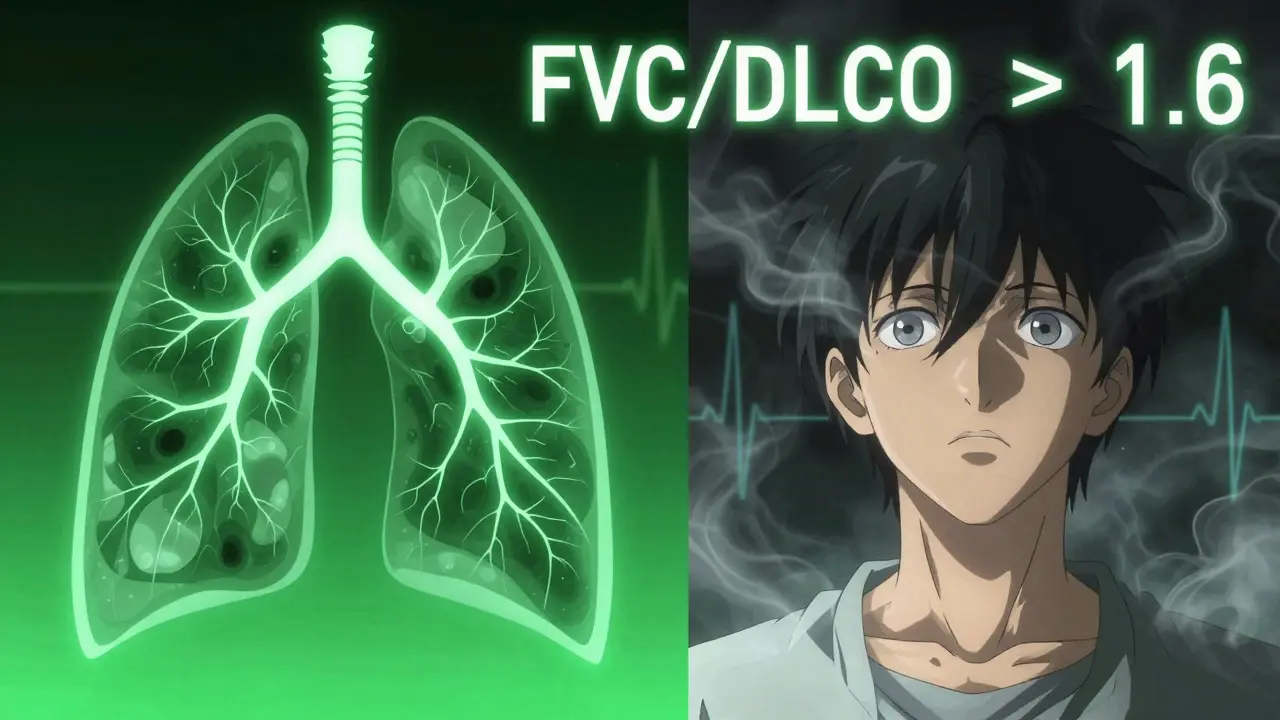
There’s also a powerful trick: the FVC/DLCO ratio. If it’s over 1.6, there’s a 92% chance you have pulmonary hypertension. That’s not something you want to miss. It’s a silent killer, and DLCO is one of the first clues.
Why DLCO Gets Ignored (And Why You Should Care)
Even among doctors, DLCO is often misunderstood. It’s not as flashy as a CT scan. It doesn’t show pictures. It gives a number. And that number depends on a few things you might not think about.
First, hemoglobin matters. If you’re anemic, your DLCO will be lower-not because your lungs are damaged, but because there’s less hemoglobin to grab the CO. Every 1 gram per deciliter drop in hemoglobin can lower DLCO by about 1%. That’s why labs must check your blood count before the test.
Second, smoking. If you smoked even a few hours before the test, your carboxyhemoglobin levels rise. That blocks CO absorption and makes DLCO look artificially low. You need to avoid smoking for at least 24 hours before the test.
Third, breath-hold timing. If you hold your breath for 8 seconds instead of 10, your result is off. The machine expects exactly 10 seconds. This is why the test isn’t always reliable in older patients or those with dementia. They can’t hold still long enough.
That’s why many clinics skip DLCO. It’s harder. But skipping it means missing early disease. And that’s dangerous.
When DLCO Changes Everything
I’ve seen cases where patients came in with worsening breathlessness. Their spirometry was normal. Their chest X-ray was clean. They were told, “You’re fine.” But their DLCO was at 58%. That’s severe.
Turns out, they had early pulmonary fibrosis. By the time their spirometry dropped, the disease was advanced. If DLCO had been done two years earlier, treatment could have slowed it down. That’s the power of this test.
DLCO is also the gold standard for tracking treatment in fibrosis. If your DLCO improves after starting a new drug, that’s real progress. If it keeps dropping, you need to change course. It’s not just a diagnosis tool-it’s a life-saving monitor.
What to Do Next
If you’ve had spirometry and your doctor hasn’t ordered DLCO, ask. Especially if:
- You have unexplained shortness of breath
- You’re being evaluated for lung surgery
- You have a connective tissue disease like scleroderma or lupus
- Your chest X-ray or CT shows abnormalities
- Your spirometry is normal but you still feel like you can’t catch your breath
Don’t assume normal spirometry means healthy lungs. It doesn’t. DLCO is the missing piece for many people. It’s not expensive-around $90 out-of-pocket in Australia-and it’s covered by Medicare if there’s a clear medical reason.
And if you’re told your DLCO is low? Don’t panic. Ask for the full picture: What’s your hemoglobin? Did you smoke recently? Is your alveolar volume normal? A good pulmonologist will look at all of it-not just the number.
These tests aren’t about fear. They’re about clarity. Knowing what’s wrong early gives you options. And options mean control.
What’s the difference between spirometry and DLCO?
Spirometry measures how much air you can move in and out of your lungs and how fast. DLCO measures how well oxygen moves from your lungs into your bloodstream. One checks airflow; the other checks gas exchange. They answer different questions.
Can DLCO be normal if I have emphysema?
Yes. In early emphysema, DLCO may be low while spirometry is still normal. But in advanced emphysema, both can be low. A normal DLCO doesn’t rule out emphysema-it just means the damage isn’t severe enough yet to affect gas transfer. A CT scan is needed to confirm.
Why does hemoglobin affect DLCO?
DLCO measures how much carbon monoxide binds to hemoglobin in your blood. If you have low hemoglobin (anemia), less CO can bind, so the test shows lower diffusion-even if your lungs are perfectly healthy. That’s why labs must check your blood count before the test.
Can I do DLCO if I have asthma?
Yes. In fact, DLCO is often normal or even high in asthma because your lungs are hyperinflated and blood flow is increased. But if your DLCO is low during an asthma flare, that suggests another problem-like early lung scarring or a blood clot. It helps separate asthma from other conditions.
How accurate is DLCO?
DLCO is highly reproducible when done correctly-within 4% of your previous result if you’re healthy. But accuracy drops if you don’t hold your breath for exactly 10 seconds, if you smoke beforehand, or if your hemoglobin isn’t measured. Follow the prep instructions carefully.
Is DLCO covered by Medicare in Australia?
Yes, if your doctor refers you with a valid reason-like unexplained breathlessness, suspected interstitial lung disease, or pre-op evaluation for lung surgery. The test is billed under MBS item 61150. You’ll usually pay nothing out-of-pocket if you have a referral.
What if my DLCO is low but I feel fine?
That’s exactly when it matters most. Many lung diseases-like early pulmonary fibrosis or small vessel disease-don’t cause symptoms until they’re advanced. A low DLCO is an early warning. It doesn’t mean you’re doomed. It means you need follow-up: a CT scan, blood tests, or repeat testing in 6 months to see if it’s getting worse.

Shanahan Crowell
January 4 2026DLCO is the silent hero of pulmonary testing-most docs skip it because it’s ‘too niche,’ but if you’re wheezing and your spirometry’s clean? That’s your wake-up call. I’ve seen people told they’re ‘just out of shape’ for years… until DLCO showed early fibrosis. Don’t let a number on a screen be your only diagnosis tool.