Pneumonia Risk Calculator
When you think of a chest infection, pneumonia probably pops up first, but the story often starts higher up-in the sinuses. A clogged, inflamed sinus can set the stage for a lung infection, and many people don’t realize the two are linked. Below we unpack how a sinus infection can lead to pneumonia, what signs to watch for, and how to keep both problems at bay.
Key Takeaways
- Pneumonia can develop after a sinus infection when germs travel down the airway.
- Both viral and bacterial agents can cause the cascade.
- Weak immunity, smoking, and chronic sinus issues raise the risk.
- Early treatment of sinus symptoms can stop a lung infection in its tracks.
- Vaccines and good nasal hygiene are the best long‑term defenses.
What Is Pneumonia?
Pneumonia is an infection that inflames the air sacs (alveoli) in one or both lungs, filling them with fluid or pus and making breathing painful. It can be triggered by bacteria, viruses, or even fungi. In the United States, about 1.5million adults are hospitalized for pneumonia each year, and the mortality rate climbs sharply for people over 65. Typical bacterial culprits include Streptococcus pneumoniae and Haemophilus influenzae, while viruses such as influenza and RSV are common in winter spikes. Symptoms range from a dry cough and fever to severe chest pain, rapid breathing, and a distinct rattling sound called rales when doctors listen with a stethoscope.
What Is a Sinus Infection?
Sinus infection (or sinusitis) is inflammation of the lining of the nasal cavities, usually caused by a virus or bacteria that blocks normal mucus drainage. It often follows a common cold, allergy flare-up, or exposure to pollutants. The blockage creates a warm, moist environment perfect for bacterial growth, leading to thick, colored discharge, facial pressure, and a reduced sense of smell. Acute sinusitis lasts less than four weeks; chronic sinusitis persists beyond three months and may require imaging studies to identify structural problems like a deviated septum or nasal polyps.
How the Two Conditions Connect
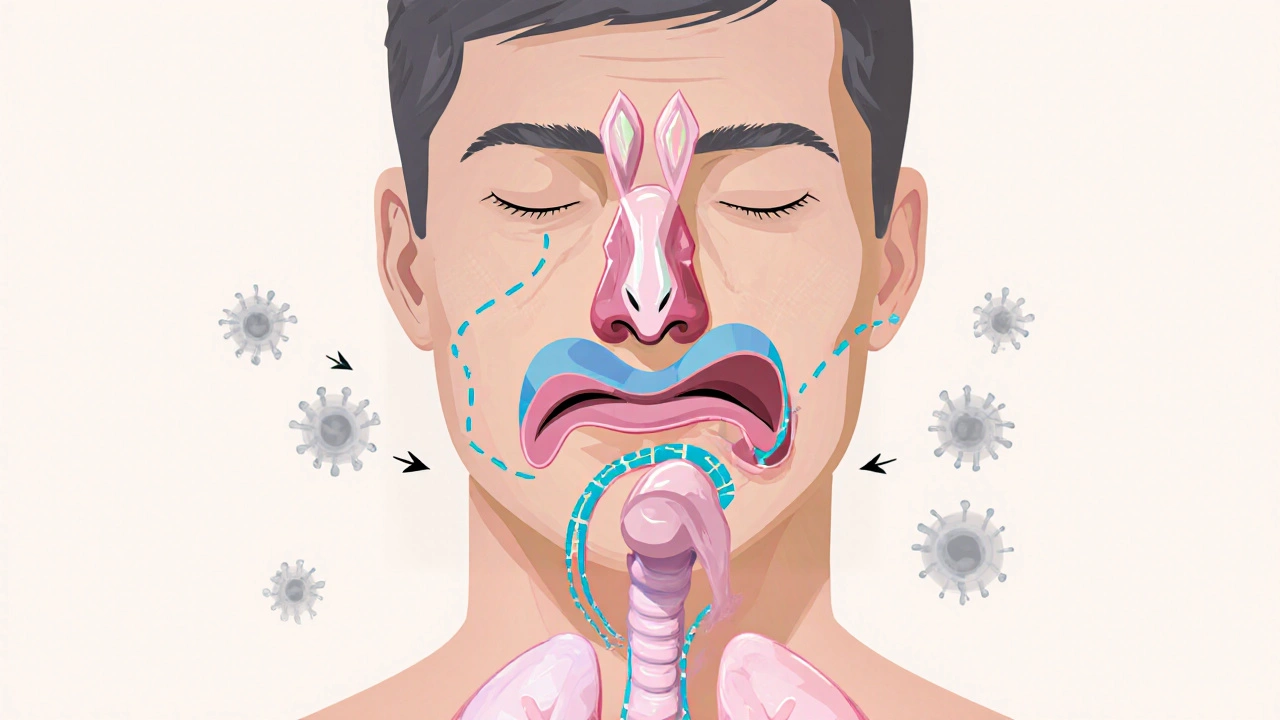
Both conditions belong to the broader family of upper respiratory tract infections. When the sinus passages are clogged, mucus can drip down the back of the throat-a process called post‑nasal drip. This drip carries microbes straight into the airway, giving them a shortcut to the lungs.
Several pathways link the infections:
- Direct spread: Bacteria such as Streptococcus pneumoniae can migrate from the nasal cavity to the bronchi, especially if the mucosal barrier is compromised.
- Immune compromise: Ongoing sinus inflammation taxes the immune system, making it less able to clear inhaled germs.
- Viral priming: A viral cold often starts in the nose, weakens the airway lining, and then a secondary bacterial infection takes hold, leading to pneumonia.
In practice, doctors see this progression more often in people who smoke, have asthma, or have untreated chronic sinusitis. Recognizing the connection early can prevent a mild sinus problem from turning into a life‑threatening lung infection.
Risk Factors & Who’s Most Susceptible
Not everyone with a runny nose ends up with pneumonia. The following factors raise the odds:
- Smoking or exposure to second‑hand smoke - it impairs ciliary action, the tiny hairs that sweep mucus out of the lungs.
- Chronic sinus problems or frequent allergic rhinitis.
- Underlying health conditions such as asthma, COPD, or diabetes.
- Age extremes - children under5 and adults over65 have weaker immune defenses.
- Recent viral illness - a flu shot can reduce the chance of a viral cascade.
People with weakened immunity, whether from medication, disease, or age, should monitor sinus symptoms closely because the barrier that normally stops germs from traveling downward is already thin.
Symptoms: Overlap and Differences
Because the two infections share a common origin, it’s easy to mix up their warning signs. The table below highlights the key overlaps and the red‑flag symptoms that point to lung involvement.
| Symptom | Typical in Sinus Infection | Typical in Pneumonia |
|---|---|---|
| Facial pressure or pain | ✔ | ✖ |
| Fever (above 38°C/100.4°F) | Occasional | Common |
| Productive cough with thick sputum | Rare | Frequent |
| Shortness of breath | ✖ | ✔ |
| Fatigue | Moderate | Severe |
| Headache | ✔ | ✖ |
Prevention Tips - Keeping Both at Bay
Stopping the chain reaction before it starts saves you a lot of trouble. Here are practical steps that work for most people:
- Vaccinate: The influenza vaccine and the pneumococcal vaccine dramatically cut the risk of viral and bacterial pneumonia.
- Practice nasal irrigation with a saline spray or neti pot to clear mucus and reduce bacterial load. Use distilled or boiled‑then‑cooled water to avoid introducing new microbes.
- Avoid smoking and limit exposure to polluted air, which impair the ciliary action in the lungs.
- Manage allergies with antihistamines or nasal steroids to keep sinus passages open, especially during pollen season.
- Maintain good hand hygiene and avoid touching your face, a simple habit that cuts down the spread of cold viruses.

When to Seek Medical Care
Most sinus infections clear up in a week or two, but certain signs mean you need a doctor’s attention:
- Fever that lasts more than three days or spikes above 39°C (102°F).
- Chest pain that worsens with deep breathing.
- Persistent cough producing green or bloody sputum.
- Rapid breathing, bluish lips, or extreme fatigue.
- Existing conditions like asthma that suddenly feel out of control.
Early diagnosis often involves a chest X‑ray and a nasal swab to pinpoint the culprit. If pneumonia is confirmed, doctors may also order blood tests to check oxygen levels and inflammation markers.
Treatment Options - From Sinus Relief to Pneumonia Care
If a sinus infection is caught early, antibiotics may be prescribed, especially when a bacterial cause is confirmed. For viral cases, decongestants, pain relievers, and rest are the mainstays. Intranasal corticosteroid sprays can reduce swelling and help mucus drain properly.
When pneumonia develops, treatment intensifies:
- Antibiotics for bacterial pneumonia - common choices include amoxicillin, macrolides, or a fluoroquinolone for resistant strains.
- Antiviral medication if flu is the trigger, such as oseltamivir, which works best when started within 48hours of symptom onset.
- Supportive care - oxygen therapy, IV fluids, and fever reducers like acetaminophen to keep you comfortable.
- Hospitalization for severe cases, especially in older adults or people with heart disease, where close monitoring of breathing and blood pressure is essential.
Completing the full course of medication, even if you feel better, prevents relapse and resistance. Follow‑up chest X‑rays are often ordered a week after treatment to ensure the infection has cleared.
Quick Checklist - What to Do If You Think the Link Is Happening
- Track symptoms daily - note fever, cough, and facial pressure.
- Start saline nasal irrigation at the first sign of congestion.
- Take an over‑the‑counter pain reliever if headache or sinus pain worsens.
- If a cough becomes productive or you develop shortness of breath, call your doctor.
- Keep your vaccinations up to date - it’s the simplest way to block the chain.
Frequently Asked Questions
Can a sinus infection cause pneumonia?
Yes. When mucus from inflamed sinuses drips down the throat, it can carry bacteria or viruses directly into the lungs, potentially leading to pneumonia, especially in people with weakened immunity.
How long does it take for a sinus infection to turn into pneumonia?
The timeline varies. In some cases, the transition can happen within a few days if the pathogen is aggressive, while other times it may take a week or more. Prompt treatment of sinus symptoms reduces the window.
Are antibiotics always needed?
No. Antibiotics are only effective against bacterial infections. Most sinus infections start as viral, so they resolve with rest, hydration, and decongestants. A doctor will prescribe antibiotics only after confirming a bacterial cause.
What vaccines help prevent this chain reaction?
The seasonal flu shot reduces viral upper‑respiratory infections, and the pneumococcal vaccine protects against the most common bacterial cause of pneumonia. Both are recommended for adults over 50 and for anyone with chronic health issues.
Is it safe to use a neti pot during a cold?
Yes, as long as you use distilled, sterile, or boiled‑then‑cooled water. Using tap water can introduce harmful organisms. A neti pot can clear mucus and lower the chance of the infection spreading to the lungs.
Understanding the pneumonia and sinus infections link gives you a clear roadmap: treat nasal congestion early, protect yourself with vaccines, and watch for lung‑related warning signs. Stay proactive, and you’ll keep both your sinuses and lungs healthy.


Stephanie Zuidervliet
October 12 2025Oh my gosh!!! The article tries to tie sinus woes to a deadly lung infection, but it feels like a rushed textbook summary, full of buzzwords and bullet points!!! Where's the real-life storytelling? I needed heart‑pounding anecdotes, not just sterile statistics!!!