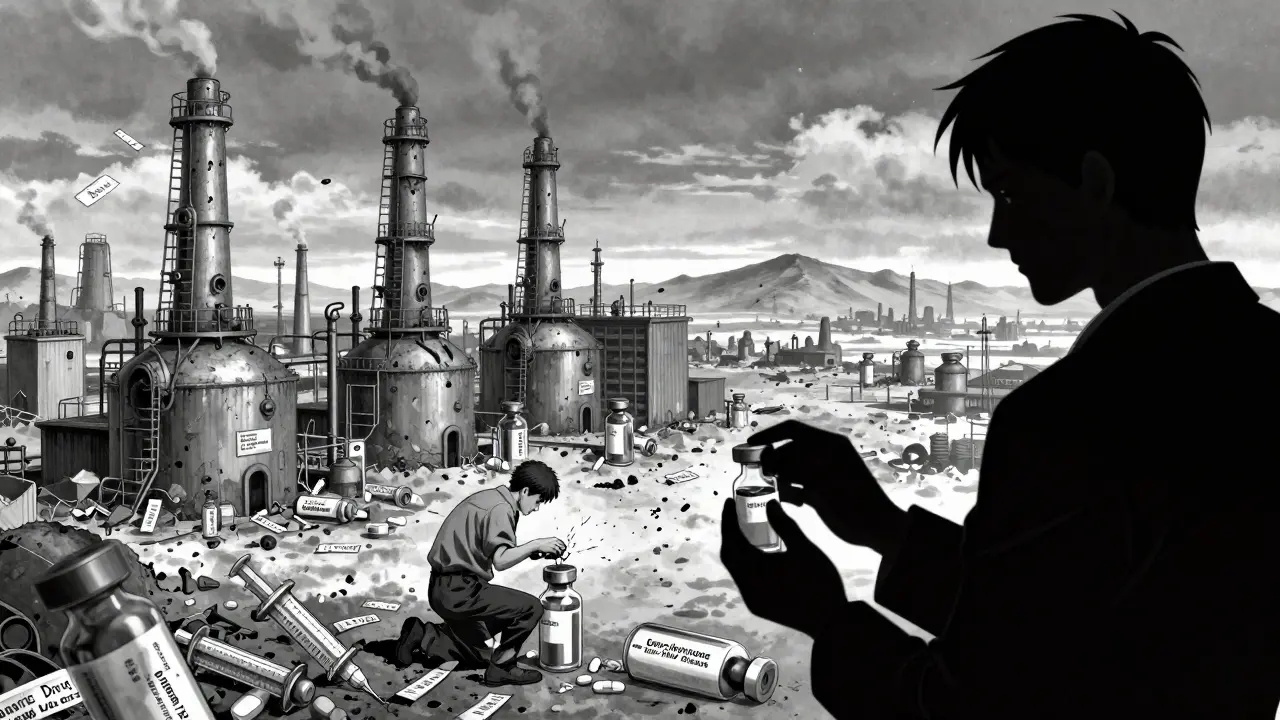
It’s 2026. You’re a nurse in a rural hospital. The IV bag of generic epinephrine your team relies on for cardiac arrests is gone. Again. The last batch expired last week. You call three distributors. None have it. The brand version costs six times more-your hospital’s budget won’t cover it. So you improvise. You use a syringe and vial, hoping the timing holds. This isn’t rare. It’s routine.
Here’s the paradox: we use generic drugs for 9 out of 10 prescriptions in the U.S. They save the system over $300 billion a year. But the very competition that makes them cheap is also making them vanish. Too many companies chasing the same low-margin drugs? That’s not helping. Too few willing to make the hard-to-produce ones? That’s the crisis.
Competition Drives Prices Down-Until It Breaks Supply
When a brand-name drug loses its patent, the race begins. Dozens of generic makers jump in. Prices drop fast. In the first year, they can fall 30-50%. By year three, with three or more competitors, prices often drop another 20%. That’s good for patients and insurers. But it’s brutal for manufacturers.
Take doxycycline, an antibiotic used for everything from acne to Lyme disease. In 2015, it cost about $1.50 per pill. By 2023, after five manufacturers entered the market, it was $0.03. One pill. Three cents. The cost to make it? Maybe two cents. Profit? Barely enough to cover shipping. So one company quits. Then another. Now only two suppliers remain. When one has a quality issue-say, a contaminated batch-the other can’t scale up fast enough. Shortage. Patients go without.
It’s not just antibiotics. Same story with metformin, levothyroxine, and hydrocortisone. These are not fancy drugs. They’re old, simple, cheap. But they’re essential. And when no one makes them, people die.
The Hidden Cost of Low Margins
Manufacturing generic drugs sounds easy. But it’s not. For simple pills, sure. But for sterile injectables-like insulin, chemotherapy drugs, or epinephrine-it’s a billion-dollar gamble. Building a clean room that meets FDA standards costs $200-500 million. The equipment alone runs $50 million. The validation process? 18 to 24 months. And you can’t just make a few batches. You need to run it 24/7 to make it profitable.
That’s why only five companies control nearly half the U.S. market for sterile injectables. They’re the only ones who can afford it. When one shuts down-like the 2023 FDA shutdown of a major epinephrine plant-there’s no backup. The FDA issued 147 warning letters to generic manufacturers in 2023 alone. That’s 23% more than the year before. Data fraud. Poor sanitation. Inadequate testing. These aren’t accidents. They’re signs of a system pushed to the edge.
Companies aren’t cutting corners because they’re greedy. They’re cutting corners because they’re broke. If you’re making a drug that sells for $0.05 a pill and your overhead is $0.04, you’re one bad batch away from bankruptcy. So you skip a test. You delay maintenance. You push production past safety limits. Then the FDA catches you. You shut down. And the shortage gets worse.
Who Makes the Drugs? It’s Not Who You Think
Most people assume U.S. companies make our generics. They don’t. Over 80% of the active ingredients in U.S. generic drugs come from India and China. And those countries aren’t just suppliers-they’re the engines of global production.
India’s Sun Pharma and Aurobindo, China’s Huahai and Zhejiang Tianyu-they’re the real powerhouses. They produce the bulk of metformin, amoxicillin, and losartan. But here’s the catch: their production is tied to volatile supply chains. A single factory fire in Shanghai can ripple across U.S. hospitals. A regulatory crackdown in India can freeze exports for months.
And when a U.S. company like Teva or Viatris sells a generic drug, they’re often just repackaging what was made overseas. They don’t own the plant. They don’t control the quality. They just get the price. And when prices collapse, they walk away. The manufacturer? They’re left holding the bag.
Why Some Drugs Have Too Few Makers
Not all generics are created equal. The market splits into two worlds:
- Simple, high-volume drugs (like ibuprofen, acetaminophen): 15-20 makers. Prices are rock bottom. Competition is fierce. But supply? Stable.
- Complex, low-margin drugs (like injectable steroids, chemotherapy agents, or older antibiotics): 1-3 makers. Prices are barely profitable. And if one leaves? Total shortage.
According to IQVIA, 35% of generic drug markets have fewer than three manufacturers. Twelve percent have just one. That’s not competition. That’s a single point of failure.
Take procainamide, a heart rhythm drug. Only one company makes it in the U.S. It’s not new. It’s not popular. But it’s life-saving for a small group of patients. No one else will make it because the market is too small. The price can’t rise. The demand is too low. So if that one plant goes dark? No backup. No alternative. Patients are stuck.
The Policy Mess: Good Intentions, Bad Outcomes
Washington keeps trying to fix this. The FDA’s Drug Competition Action Plan has approved 40% more first generics since 2017. Great, right? Not quite. More approvals mean more companies chasing the same low-margin drugs. That drives prices even lower. And more companies mean more inspections-and more shutdowns.
Then there’s the Inflation Reduction Act. Starting in 2026, Medicare will negotiate prices for 10 high-cost drugs. That’s good for seniors. But it’s bad for generics. Why? Because the negotiated price becomes the new benchmark. If Medicare pays $2 for a drug, private insurers will demand the same. Manufacturers who were barely scraping by now face 15-25% margin cuts. Many will quit.
The European Medicines Agency got it right: for essential medicines, you need 4-6 manufacturers. Enough to keep prices low. Enough to ensure backup. But right now, only 65% of essential generics meet that standard. The rest? One or two makers. One shutdown. No supply.

What’s Really Going On? A System Designed to Fail
We’ve built a system that rewards the lowest price above all else. We don’t care how many companies make a drug. We don’t care if they’re financially stable. We don’t care if they have a backup plan. We just want the cheapest pill on the shelf.
But drugs aren’t toothpaste. You can’t just switch brands when the supply runs out. A patient on levothyroxine can’t suddenly switch to a different generic without risking their thyroid levels. Even tiny differences in inactive ingredients can cause problems. So when the supply vanishes, they don’t get a substitute. They get silence.
Meanwhile, the companies that make the complex, high-risk drugs-sterile injectables, biosimilars, oncology generics-are the ones that survive. Why? Because they’re harder to copy. Fewer players. Higher margins. But they’re not making the everyday drugs we all need.
There’s a Better Way
We don’t need more competition. We need smarter competition.
- Guaranteed minimum volumes for essential drugs. If a hospital needs 100,000 vials of epinephrine a year, the government should contract with at least three manufacturers to produce them-no bidding wars, just steady orders.
- Strategic stockpiles for critical generics. Not just for pandemics. For everyday shortages. Like the U.S. Strategic National Stockpile, but for metformin, insulin, and antibiotics.
- Profitability thresholds. Set a floor. If a drug’s price falls below the cost of safe, compliant manufacturing, the government steps in to subsidize production until a second maker enters.
- Regional manufacturing hubs. Invest in U.S.-based sterile injectable facilities-not to replace India, but to ensure backup capacity. The U.S. can’t be 100% dependent on foreign supply for life-saving drugs.
This isn’t about protecting profits. It’s about protecting patients. We don’t need 20 companies making the same $0.02 pill. We need 4 reliable ones making the $1.50 drug that no one else wants to touch.
What Happens If We Don’t Change?
By 2029, biosimilars will drive $217 billion in new generic growth. That’s good news for cancer patients. But it’s bad news for the rest of us. The market will keep shifting toward high-margin, complex drugs. The simple, old, cheap ones? They’ll keep disappearing.
More shortages. More delays. More patients going without. More doctors improvising. More families paying out of pocket for brand-name drugs they can’t afford.
We’ve optimized for price. We’ve forgotten about resilience. We’ve forgotten about safety. We’ve forgotten that a drug isn’t just a chemical. It’s a lifeline.
The next time you hear a politician talk about lowering drug prices, ask this: “At what cost?”


Kelly McRainey Moore
January 21 2026Man, I just saw a nurse post on Instagram about having to use a syringe for epinephrine during a code. I cried. These aren’t just drugs-they’re lifelines. And we treat them like commodities.