Gabapentinoid-Opioid Risk Assessment Tool
Calculate Your Risk
This tool estimates your risk of respiratory depression when taking both a gabapentinoid and an opioid. Your results will help you discuss safer pain management options with your doctor.
When you’re in chronic pain, doctors often turn to gabapentinoids like gabapentin or pregabalin to help manage nerve pain. At the same time, opioids like oxycodone or morphine are prescribed for severe pain. It seems logical-combine them, and you get better pain control. But what many don’t realize is that this combination can slow your breathing to a dangerous level, even stop it completely. This isn’t a rare side effect. It’s a well-documented, life-threatening interaction that’s been quietly killing people for years.
The Science Behind the Risk
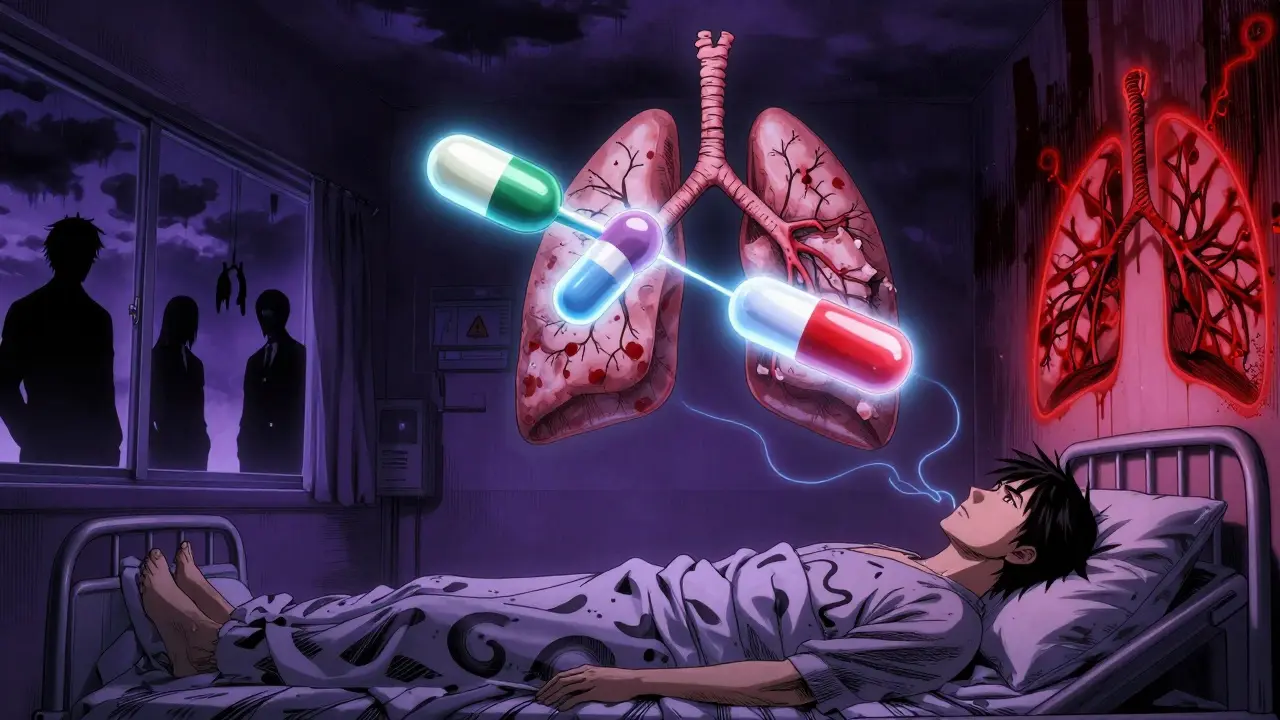
Gabapentinoids work by calming overactive nerves, which helps with conditions like diabetic neuropathy, postherpetic neuralgia, and some types of seizures. But they also affect the brainstem-the part that controls breathing. Alone, they can cause mild respiratory depression, especially in older adults or those with lung disease. But when you add an opioid, the effect isn’t just added-it’s multiplied. A 2017 study in PLOS Medicine followed over 16 years of prescription data and found that patients taking both gabapentin and opioids had a 50% higher risk of dying from an opioid overdose. For those on high doses of gabapentin, the risk jumped nearly double. That’s not a small increase. That’s a major red flag. The mechanism isn’t just about both drugs slowing breathing. Gabapentinoids can reverse opioid tolerance. That means someone who’s been on opioids for months and built up a tolerance might suddenly become sensitive again when gabapentin is added. Their body, used to higher opioid levels, now reacts like they’re taking a brand-new dose. This can trigger sudden, fatal respiratory failure-even if they’ve been stable for years.Who’s Most at Risk?
It’s not just anyone. Certain people are far more vulnerable:- People over 65: Aging lungs and slower metabolism make it harder to clear these drugs. Brainstem sensitivity also increases with age.
- Those with COPD, sleep apnea, or asthma: Their breathing is already compromised. Adding a CNS depressant pushes them past their limit.
- Patients with kidney problems: Both gabapentin and pregabalin are cleared by the kidneys. If kidney function is low, the drugs build up in the blood, increasing toxicity.
- People on high doses: Doses above 1,800 mg/day of gabapentin or 300 mg/day of pregabalin significantly raise the risk.
- Post-surgery patients: One study of over 5.5 million surgical patients found respiratory depression rates as high as 72% in general surgery when gabapentinoids were used with opioids.
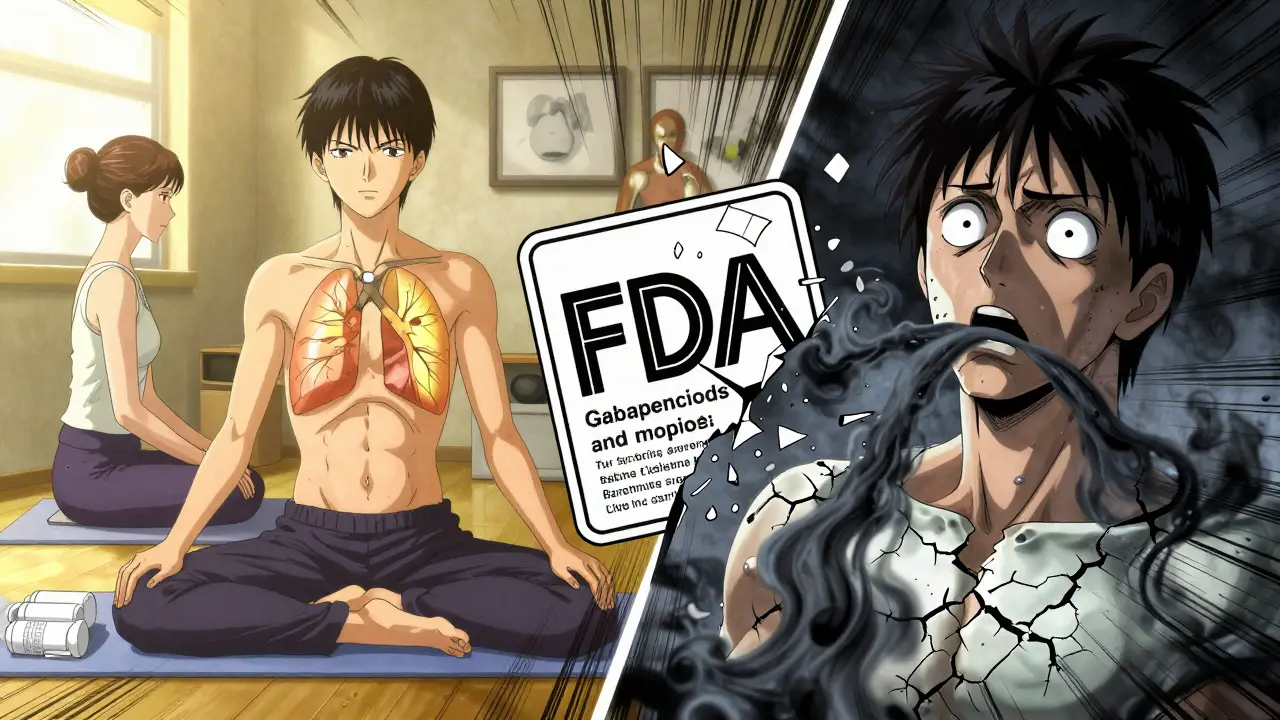
What the Regulators Say
In April 2019, the U.S. Food and Drug Administration (FDA) issued a formal warning after reviewing over 49 cases of respiratory depression linked to gabapentinoids. Of those, 24% ended in death-and every single fatal case involved either an opioid, another CNS depressant, or an underlying health condition like lung disease. The UK’s Medicines and Healthcare products Regulatory Agency (MHRA) followed with a similar alert. Both agencies required label changes on all gabapentinoid products. The new warnings now clearly state: “Gabapentinoids can cause respiratory depression, especially when combined with opioids.” Despite this, co-prescribing remains common. In 2017, nearly 1 in 5 new gabapentin prescriptions came with an opioid. Many doctors still see gabapentinoids as a safe alternative to opioids. But the data shows the opposite: they’re not replacing risk-they’re compounding it.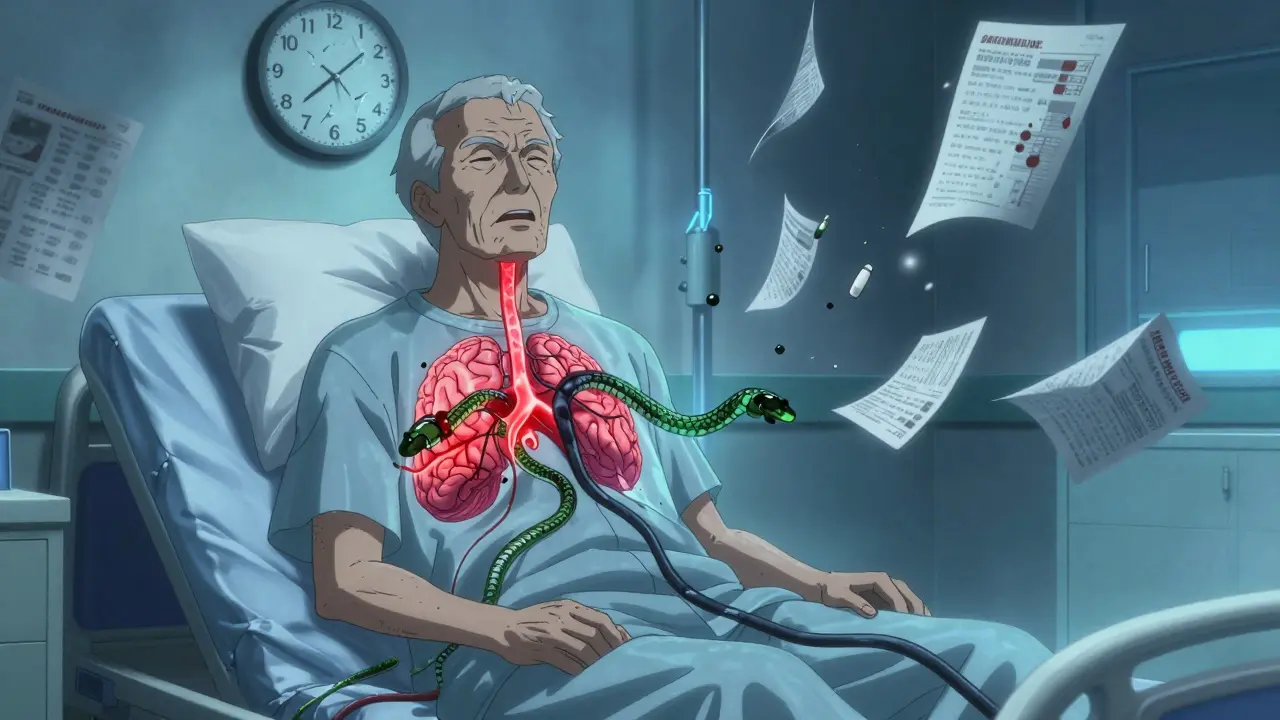
Why Do Doctors Still Prescribe Them Together?
The answer lies in a well-intentioned but flawed assumption: that gabapentinoids reduce opioid use. Many clinicians believe adding gabapentin lets them lower opioid doses, making treatment safer. But the evidence doesn’t back this up. A 2020 analysis in JAMA Network Open found no clear benefit to combining gabapentinoids with opioids for postoperative pain. In fact, the added risk of respiratory depression often outweighs any minor pain relief gain. For many patients, gabapentinoids don’t make opioids more effective-they just make them deadlier. The rise in gabapentinoid use after the CDC’s 2016 opioid guidelines didn’t reduce opioid deaths. It just shifted the danger. Instead of overdosing on opioids alone, people are now overdosing on the combo.What Should You Do If You’re Taking Both?
If you’re currently on both gabapentinoids and opioids, don’t stop suddenly. Withdrawal from either can be dangerous. But you need to talk to your doctor-right away. Ask these questions:- Is this combination still necessary for my pain control?
- Have my kidney function and lung health been checked recently?
- Can we try tapering one of these medications, starting with the gabapentinoid?
- Are there safer alternatives for my type of pain-like physical therapy, non-opioid analgesics, or nerve blocks?
What Are the Alternatives?
There are other ways to manage neuropathic pain without risking your breathing:- Duloxetine and venlafaxine: These antidepressants are FDA-approved for diabetic nerve pain and don’t affect breathing.
- Topical lidocaine or capsaicin: Useful for localized pain, with no systemic side effects.
- Cognitive behavioral therapy (CBT): Proven to reduce pain perception and improve quality of life without drugs.
- Physical therapy and exercise: Especially effective for chronic back and joint pain.
- Non-opioid analgesics: Like acetaminophen or NSAIDs (if safe for your stomach and kidneys).
The Bigger Picture
This isn’t just about two drugs. It’s about how we treat pain in modern medicine. We’ve been trained to reach for pills first. But when those pills interact in deadly ways, we need to rethink our approach. The fact that this interaction was known for years-and still continues-is a failure of clinical practice, not science. We have the data. We have the warnings. What’s missing is the urgency. If you’re taking gabapentinoids with opioids, you’re not just managing pain-you’re playing Russian roulette with your breathing. The odds aren’t in your favor. And unlike a game, you can’t restart.What to Watch For
If you or someone you know is on this combo, learn the warning signs of respiratory depression:- Shallow or slow breathing (fewer than 10 breaths per minute)
- Feeling unusually drowsy or hard to wake up
- Confusion, dizziness, or slurred speech
- Lips or fingertips turning blue
- Unresponsiveness
Can gabapentin or pregabalin cause respiratory depression on their own?
Yes. While the risk is higher when combined with opioids, gabapentinoids alone can cause respiratory depression, especially in older adults, people with lung disease, or those with kidney impairment. The FDA reviewed cases where respiratory depression occurred even with gabapentinoid monotherapy, and some resulted in death.
How common is it for doctors to prescribe gabapentinoids with opioids?
Very common. In 2017, nearly 22% of new gabapentin prescriptions and 24% of new pregabalin prescriptions were given alongside opioids. This practice continues despite FDA and MHRA warnings. Many doctors still believe gabapentinoids reduce opioid doses, but studies show this benefit is minimal-and the risk is high.
Are there any safe doses of gabapentinoids when taking opioids?
There’s no completely safe dose when combining these drugs. The risk increases with higher doses and in vulnerable populations. The safest approach is to avoid the combination entirely unless no other options exist-and even then, use the lowest possible dose of both, with close monitoring.
Can I stop taking gabapentin if I’m on opioids?
Don’t stop abruptly. Suddenly stopping gabapentin can cause seizures, anxiety, or insomnia. Talk to your doctor about a slow, supervised taper. The same applies to opioids-never stop them cold turkey. A phased reduction under medical supervision is essential.
Why wasn’t this risk known sooner?
Gabapentinoids were initially thought to be safer than opioids because they don’t bind to opioid receptors. Their respiratory effects were underestimated, especially in real-world use. Large population studies like the 2017 PLOS Medicine analysis were needed to reveal the true scale of the danger. Regulatory agencies only acted after dozens of deaths were reported.

Lydia H.
January 19 2026Been on gabapentin for neuropathy for five years. My doc added oxycodone after a bad back surgery. I didn’t realize how dangerous it was until I started nodding off mid-conversation. Scary stuff. I’m tapering off the gabapentin now-felt like I was sleepwalking through life.
Wish I’d known this sooner.