Beta-Blocker Exercise Intensity Tool
How to Measure Your Effort
Choose the method recommended in the article for accurate exercise intensity monitoring on beta-blockers:
Your Safe Exercise Intensity
When you're on beta-blockers, your body doesn't respond to exercise the way it used to. You might feel like you're working just as hard, but you're not getting the same results. Your heart doesn't race like it used to. You get tired faster. You might even notice you're not sweating as much - even when you're walking uphill. This isn't laziness. It's pharmacology.
Why Beta-Blockers Make Exercise Feel Harder
Beta-blockers like metoprolol, propranolol, and atenolol are designed to slow your heart rate and lower blood pressure. That’s great for your heart if you have high blood pressure, angina, or heart failure. But it also means your body can’t ramp up its effort during physical activity the way it normally would.
Your heart rate during exercise is usually a reliable indicator of how hard you’re working. On beta-blockers, that’s broken. Research shows these drugs reduce your maximum heart rate by 20-30%. So if you used to hit 170 bpm during a run, you might now max out at 130 - even if you’re pushing yourself to the limit. That drop directly reduces how much oxygen your muscles get. Less oxygen means less energy. And that’s why you hit the wall sooner.
It’s not just your heart. Beta-blockers also blunt your body’s ability to tap into stored sugar for quick energy. Adrenaline normally helps release glucose during exertion, but these drugs block that signal. So even if you’re fit, your muscles feel like they’re running on empty.
How Other Medications Compare
Not all heart medications affect exercise the same way. ACE inhibitors like lisinopril or calcium channel blockers like amlodipine don’t limit your heart rate. They might cause leg swelling or dizziness, but they won’t make you feel like you’re running in slow motion. Diuretics can mess with your electrolytes and cause cramps, but they don’t cap your heart rate like beta-blockers do.
The biggest difference? Beta-blockers directly shut down your heart’s ability to respond to effort. That’s why heart rate monitors become useless on these drugs. Trying to hit your old target heart rate doesn’t just feel frustrating - it’s dangerous. You could push too hard without realizing it.
Stop Tracking Heart Rate. Start Tracking How You Feel.
If you’re on beta-blockers, forget your fitness tracker’s heart rate zones. They’re not accurate for you. Instead, use the talk test.
Here’s how it works: if you can talk comfortably during exercise - not sing, but hold a conversation - you’re in the right zone. If you’re gasping for words after every sentence, you’re going too hard. This simple rule is backed by the American Heart Association and has been proven more reliable than heart rate for people on beta-blockers.
Another tool is the Borg Rating of Perceived Exertion (RPE) scale. It runs from 6 (no effort) to 20 (max effort). Aim for 12-14 for moderate exercise - that’s “somewhat hard.” You should feel challenged, but not exhausted. Many people on beta-blockers find they need to reduce their target RPE by one level compared to before they started the medication.

How to Adjust Your Workouts
You don’t have to stop exercising. You just have to change how you do it.
- Extend your warm-up. Instead of 5 minutes, spend 10-15 minutes easing into your workout. Your heart needs more time to adjust.
- Go longer, not harder. If you used to run for 30 minutes, try 40-45. The American Heart Association recommends 180-188 minutes of moderate activity per week for beta-blocker users - up from the standard 150.
- Swap HIIT for steady, controlled intervals. High-intensity interval training (HIIT) can be risky. Your heart can’t spike fast enough to benefit from short bursts. Instead, try 2 minutes of moderate effort followed by 1 minute of rest. Repeat 5-8 times. This pattern has been shown to improve endurance better than continuous jogging for people on beta-blockers.
- Adjust strength training. Beta-blockers don’t weaken your muscles - they just limit your heart’s ability to support them. Lower the weight by 15-20%, but keep the reps the same. Focus on control, not max lifts.
Watch for Warning Signs
Fatigue is normal. Danger isn’t.
Pay attention to these red flags:
- Your resting heart rate drops below 45 bpm and you feel dizzy or lightheaded.
- Your systolic blood pressure falls below 90 mmHg during exercise.
- You’re not sweating at all during mild activity - even in warm weather. This can signal dehydration, which is more dangerous when your body can’t regulate temperature properly.
- You feel chest pain, pressure, or extreme shortness of breath that doesn’t go away after stopping.
If any of these happen, stop exercising and contact your doctor. These aren’t normal side effects - they’re signals your body is under too much stress.
Real People, Real Adjustments
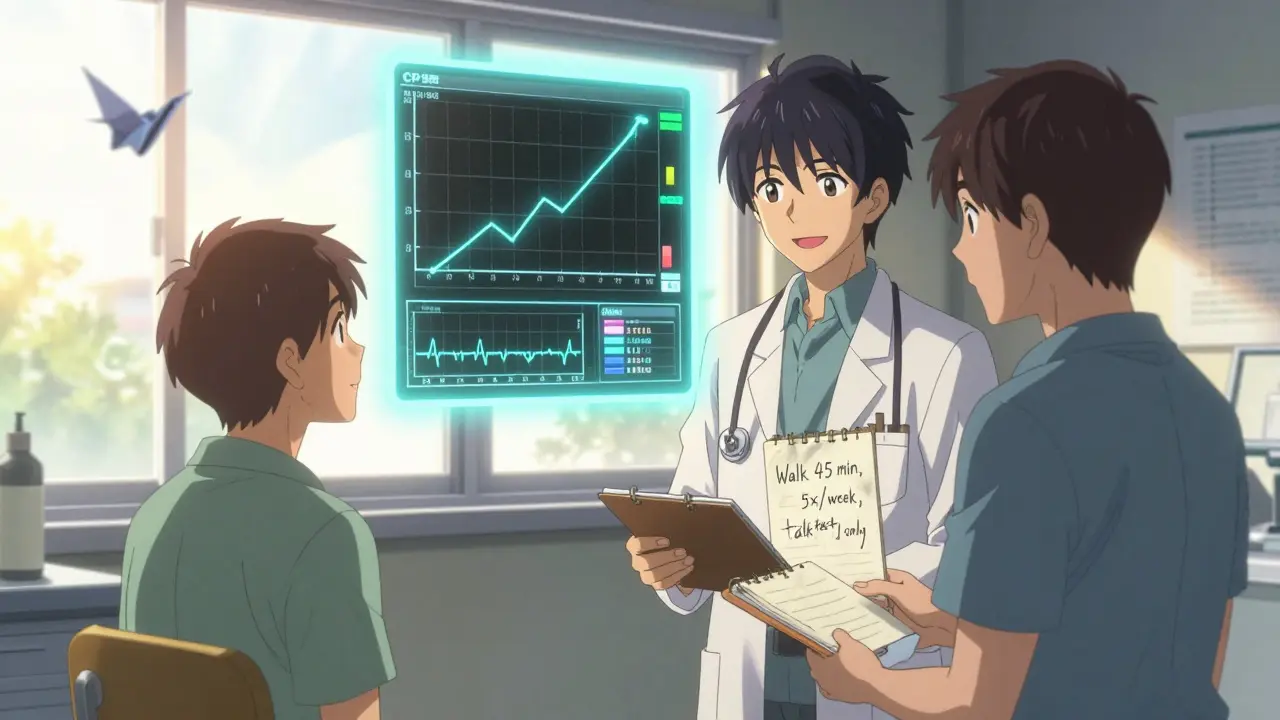
One user on Reddit, on 100mg of metoprolol, noticed his 5K time went from 25:30 to 29:15 - a 15% drop - even though he felt like he was trying just as hard. He didn’t quit. He switched from tracking pace to using the talk test. Now he walks briskly for 45 minutes, five days a week. He says he feels stronger than he has in years.
Another user on the American Heart Association’s support forum switched from atenolol to nebivolol, a newer beta-blocker that has less impact on oxygen use. She noticed she could walk longer without stopping. Her doctor didn’t change her dose - just the drug. That’s an option worth discussing if you’re struggling.
The Future Is Personalized
Doctors are starting to use cardiopulmonary exercise testing (CPET) to tailor exercise plans for people on beta-blockers. This test measures exactly how much oxygen your body uses during activity - giving a real picture of your limits, not guesses based on heart rate.
Some smartwatches now include beta-blocker-adjusted heart rate zones in their software. Apple Watch’s latest update (version 9.1) tries to account for medication effects, but it’s still experimental. Don’t rely on it yet. Use your body’s signals instead.
The goal isn’t to run like you did before. It’s to stay strong, healthy, and active - safely - for years to come. That’s possible. You just need to listen to your body, not your watch.
Can I still run on beta-blockers?
Yes, but you’ll need to adjust your pace and expectations. Your heart rate won’t rise as high, so don’t chase old numbers. Use the talk test or Borg RPE scale to gauge effort. Many people continue running - just slower and for longer durations. Focus on consistency, not speed.
Why am I not sweating even when I’m working out?
Beta-blockers can reduce sweat production because they block adrenaline, which normally triggers sweat glands. This doesn’t mean you’re not working hard - it just means your body’s cooling system is dampened. Drink water regularly, even if you don’t feel thirsty. Dehydration can be dangerous without the usual warning signs.
Should I stop beta-blockers to exercise better?
Never stop or change your medication without talking to your doctor. Beta-blockers protect your heart. The benefits usually outweigh the exercise limitations. Instead of stopping, adjust your workouts. Many people find they can stay active and healthy while staying on their meds - they just need to change how they train.
Is walking enough if I can’t run?
Absolutely. Walking is one of the best exercises for people on beta-blockers. It’s low impact, easy to control, and highly effective for heart health. Aim for 45-60 minutes, 5 days a week. Use the talk test to keep intensity moderate. You’ll improve endurance, lower blood pressure, and reduce fatigue over time - all without overloading your heart.
Can I use a fitness tracker at all?
You can use it for step count, duration, and calories burned - but ignore the heart rate zone alerts. They’re designed for people not on beta-blockers and will mislead you. Use your watch to track time and movement, not effort. Let your breathing and ability to talk be your guide.
What if I feel more tired even after adjusting my routine?
Fatigue can also come from low iron, thyroid issues, or other medications. Talk to your doctor about checking your iron levels, thyroid function, and reviewing all your prescriptions. Sometimes switching to a more selective beta-blocker like nebivolol helps. Don’t assume it’s just the drug - get a full check-up.


Ashlee Montgomery
January 10 2026It’s wild how much our bodies adapt when we stop chasing numbers and start listening. I’ve been on metoprolol for three years now. My watch still shows my heart rate at 125 during walks, but I don’t care anymore. If I can talk to my neighbor without gasping, I’m good. No more chasing ghosts of my old self.