If you’re wondering whether Entocort is the right choice for your inflammatory bowel disease, you’re not alone. Patients and doctors constantly weigh its benefits against a growing list of alternatives, from other steroids to cutting‑edge biologics. This guide breaks down the most important factors - efficacy, safety, dosing, cost and convenience - so you can see exactly where Entocort stands.
What is Entocort?
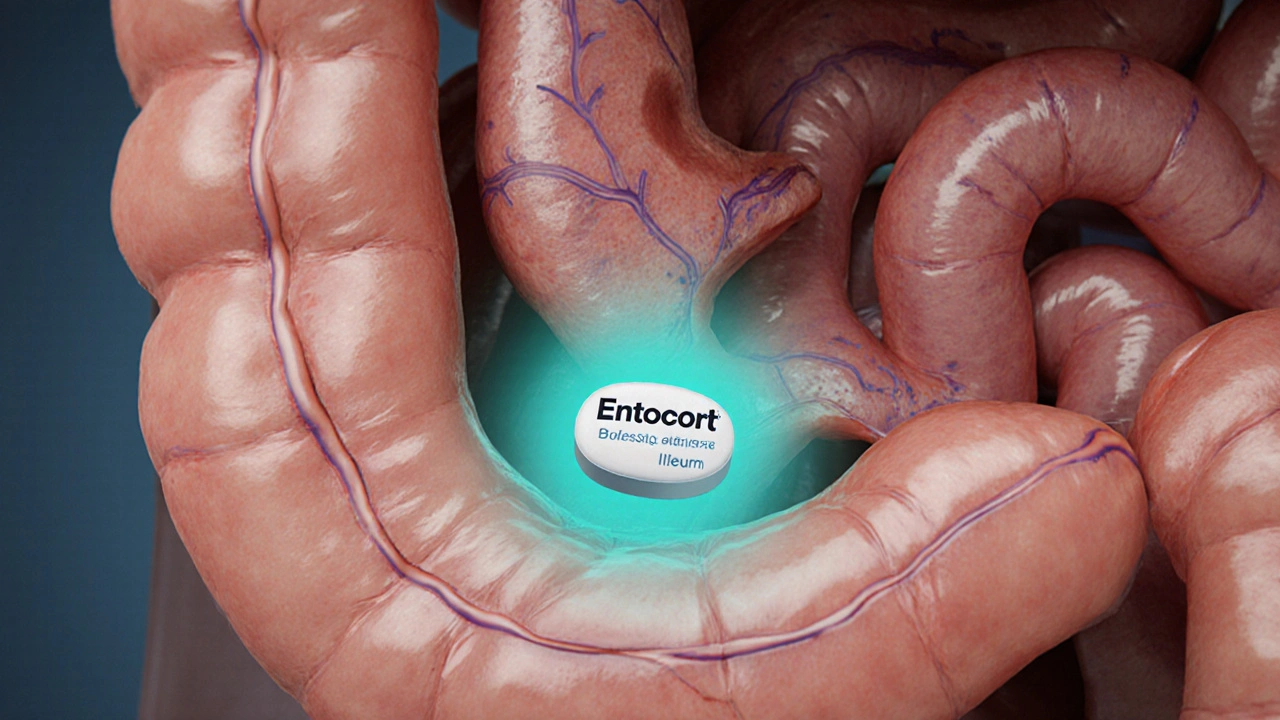
Entocort is a delayed‑release tablet that contains budesonide, a synthetic glucocorticoid. It is formulated to dissolve in the ileum and colon, delivering high local concentrations while keeping systemic exposure low. FDA‑approved for mild‑to‑moderate Crohn’s disease affecting the ileum and right colon, it comes in 3mg and 9mg strengths and is taken once daily.
How Budesonide Works
The active ingredient binds to glucocorticoid receptors in intestinal immune cells, suppressing cytokine production and reducing inflammation. Because the tablet is coated with a pH‑dependent polymer, most of the drug bypasses the stomach and releases in the lower gut, which is why side‑effects such as weight gain or bone loss are typically less severe than with systemic steroids.
Key Decision Factors
When comparing any IBD therapy, keep these five pillars in mind:
- Clinical efficacy - remission rates and time to symptom relief.
- Safety profile - short‑ and long‑term adverse events.
- Dosing convenience - frequency, route (oral, injection, infusion).
- Cost & insurance coverage - out‑of‑pocket expense for patients in Australia and abroad.
- Patient suitability - disease location, severity, comorbidities.

Top Alternatives to Entocort
Below is a quick snapshot of the most widely used alternatives, each introduced with its own schema markup for easy indexing.
Prednisone - a classic oral glucocorticoid with systemic action. It works quickly but carries higher risks of weight gain, mood swings, and bone loss. Often reserved for short‑term flare control.
Mesalamine (5‑ASA) - an anti‑inflammatory compound that stays in the gut lumen. Ideal for mild ulcerative colitis, but less effective for Crohn’s disease involving the small intestine.
Azathioprine - an immunomodulator that reduces immune cell proliferation. Takes weeks to months to become effective; useful for maintaining remission, especially when steroids are being tapered.
Infliximab - a monoclonal antibody that neutralizes tumor necrosis factor‑α (TNF‑α). Administered by IV infusion every 6-8 weeks, it offers high remission rates for moderate‑to‑severe Crohn’s and ulcerative colitis but requires pre‑screening for infections.
Vedolizumab - an integrin antagonist that blocks gut‑specific leukocyte trafficking. Given by IV infusion, it boasts a gut‑selective safety profile, making it attractive for patients concerned about systemic immunosuppression.
Ustekinumab - a human antibody targeting interleukin‑12/23. Available as subcutaneous injection after an initial IV dose; effective for both Crohn’s disease and ulcerative colitis, especially in biologic‑experienced patients.
Budesonide Controlled‑Release (Entocort EC) - 9mg - a higher‑dose version used when 3mg fails to induce remission. Still retains the low‑systemic‑exposure advantage.
Side‑by‑Side Comparison Table
| Attribute | Entocort (Budesonide) | Prednisone | Mesalamine | Azathioprine | Infliximab | Vedolizumab | Ustekinumab |
|---|---|---|---|---|---|---|---|
| Route | Oral tablet | Oral tablet | Oral/rectal | Oral | IV infusion | IV infusion | IV then SC injection |
| Target disease | Crohn’s (ileum/right colon) | All IBD flares | Ulcerative colitis (mild‑moderate) | Maintenance therapy | Moderate‑severe Crohn’s/UC | Moderate‑severe IBD | Moderate‑severe IBD (biologic‑experienced) |
| Remission rate (clinical trials) | ≈55% (8weeks) | ≈45% (4weeks) | ≈30% (8weeks) | ≈45% (12weeks) | ≈65% (12weeks) | ≈60% (12weeks) | ≈62% (12weeks) |
| Common side‑effects | Mild nausea, headache | Weight gain, hyperglycemia | Headache, nausea | Liver enzyme rise, leukopenia | Infusion reactions, infections | Upper‑respiratory infections | Injection site pain, infections |
| Systemic steroid exposure | Low (first‑pass metabolism) | High | None | None | None | None | None |
| Typical cost (AU$ per month) | ≈$120 | ≈$30 | ≈$45 | ≈$80 | ≈$1,800 | ≈$1,500 | ≈$1,600 |
| Insurance coverage (Australia) | Pharmaceutical Benefits Scheme (PBS) listed | PBS listed | PBS listed | PBS listed | Limited to specialist‑prescribed cases | Limited to specialist‑prescribed cases | Limited to specialist‑prescribed cases |

Which Option Fits Your Situation?
1. Mild ileal Crohn’s disease, no prior steroid exposure - Entocort’s targeted release makes it a first‑line oral choice. Its low systemic absorption keeps side‑effects minimal.
2. Acute severe flare, any disease location - Prednisone or a short burst of intravenous steroids is faster acting, though you’ll need a taper plan to avoid rebound inflammation.
3. Ulcerative colitis limited to the colon - Mesalamine is cheap, well‑tolerated, and works well for mild‑to‑moderate disease.
4. Need for long‑term steroid sparing - Azathioprine or mercaptopurine are the go‑to immunomodulators; they take weeks to kick in but help keep you off steroids.
5. Moderate‑to‑severe disease unresponsive to steroids - Biologics (Infliximab, Vedolizumab, Ustekinumab) are the most effective. Choice depends on infection risk, patient preference for infusion versus injection, and prior biologic exposure.
Practical Tips & Common Pitfalls
- Always take Entocort with a full glass of water on an empty stomach; food can delay release and lessen efficacy.
- Check bone density after six months of any steroid, even low‑dose budesonide, especially in post‑menopausal women.
- If you’re switching from prednisone to Entocort, follow a taper schedule to avoid adrenal insufficiency.
- Biologics require pre‑infusion screening for TB and hepatitis; keep vaccination records up to date.
- For patients on azathioprine, TPMT enzyme testing before start can prevent severe bone‑marrow toxicity.
Frequently Asked Questions
Can I take Entocort and a probiotic at the same time?
Yes. Probiotics act in the gut lumen and don’t interfere with budesonide’s anti‑inflammatory action. Many clinicians recommend a daily probiotic to support microbiome health while you’re on medication.
How long should I stay on Entocort before considering a switch?
Clinical trials show that an 8‑week course is enough to judge response. If symptoms persist after that period, discuss stepping up to a higher‑dose budesonide or another class with your gastroenterologist.
Is Entocort safe during pregnancy?
Budesonide is classified as Pregnancy Category B in Australia, meaning animal studies have not shown risk and there are no well‑controlled human studies. Most specialists consider it acceptable when the benefits outweigh potential risks.
Why is Entocort cheaper than biologics?
It’s a small‑molecule oral tablet manufactured at scale, whereas biologics are large‑molecule proteins requiring complex biologic production and cold‑chain logistics. Those manufacturing differences drive the price gap.
What should I do if I miss a dose of Entocort?
Take the missed tablet as soon as you remember, unless it’s close to the next scheduled dose. In that case, skip the missed one and continue with your regular timing; don’t double up.

Marc Clarke
October 12 2025Honestly, budesonide’s low‑systemic profile makes it feel like the go‑to for mild ileal Crohn’s, especially when you want to dodge the classic steroid baggage. Take it with water on an empty stomach, and you’ll often see a decent swing in symptoms within a few weeks. It’s not a miracle cure, but it’s a solid middle ground between over‑the‑counter stuff and big‑ticket biologics. Plus, the PBS coverage in Australia keeps the out‑of‑pocket cost reasonable.