When your doctor says you need an ECG or a stress test, it’s not just another checkbox. It’s a clear signal they’re looking closely at your heart - not because something’s definitely wrong, but because they want to be sure. These tests are simple, non-invasive, and among the most common ways doctors catch heart problems before they become emergencies. If you’ve ever felt chest tightness, gotten winded climbing stairs, or have a family history of heart disease, understanding what these tests do - and what they don’t - can take the fear out of the process.
What an ECG Actually Measures
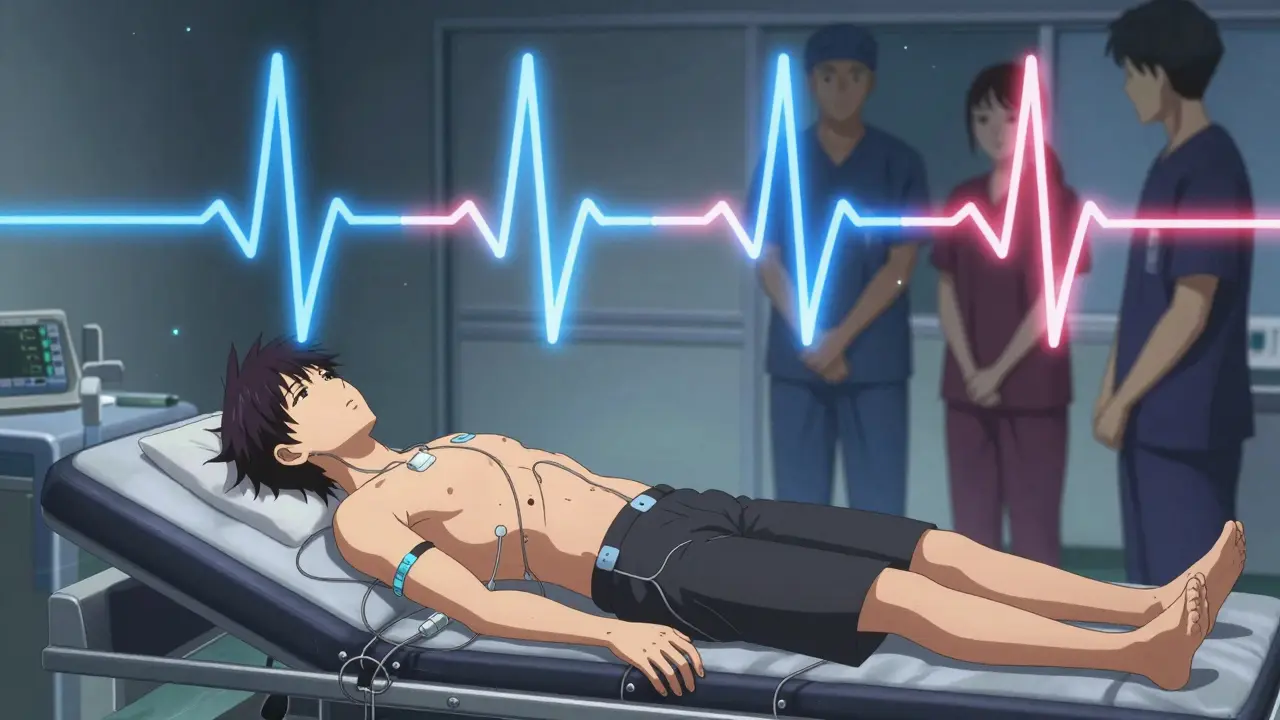
An electrocardiogram, or ECG (also called EKG), records the electrical signals that make your heart beat. It doesn’t check for blocked arteries directly. Instead, it shows how fast your heart is beating, whether the rhythm is steady, and if there’s any damage from a past heart attack. The test takes less than five minutes. You lie down, small sticky patches (electrodes) are placed on your chest, arms, and legs, and a machine draws a line graph of your heart’s electrical activity.That graph - the squiggly lines on paper or screen - tells doctors if your heart’s wiring is working right. A flat line where there should be a spike? That could mean a heart attack happened. Irregular spikes? It might be an arrhythmia. A slow or fast rhythm? That’s also visible. ECGs are quick, painless, and safe. They don’t use radiation. They don’t require fasting. You can walk in, get tested, and walk out.
But here’s the catch: a normal ECG doesn’t mean your heart is perfectly healthy. Many people with early-stage coronary artery disease have perfectly normal resting ECGs. That’s why doctors sometimes ask for more - especially if you have symptoms like chest pain during activity or unexplained shortness of breath.
Why You Might Need a Stress Test
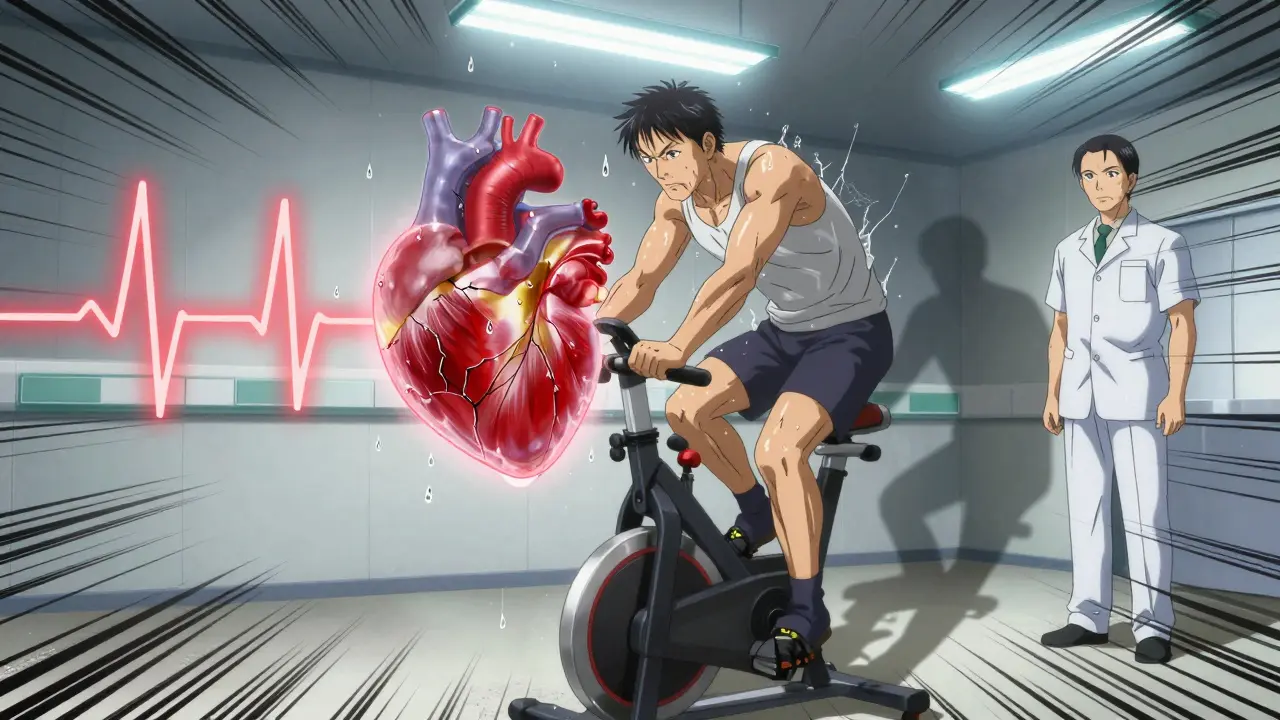
A stress test answers a different question: How does your heart handle being pushed? Most heart problems only show up when the heart is working hard. That’s why a resting ECG might look fine, but your heart struggles during exercise.The most common type is the exercise stress test. You walk on a treadmill or pedal a stationary bike while your heart rate, blood pressure, and ECG are monitored. The speed and incline increase every few minutes - slowly, but steadily - until you’re breathing hard or your heart hits its target rate. That target? Usually 85% of 220 minus your age. So if you’re 55, your max target is about 144 beats per minute.
The goal isn’t to make you collapse. It’s to see if your heart gets enough blood when it’s under pressure. If your ECG shows abnormal patterns during exercise - like dips in the ST segment - it could mean parts of your heart aren’t getting enough oxygen. That’s often a sign of narrowed arteries from plaque buildup, known as coronary artery disease.
But not everyone can run on a treadmill. If you have arthritis, severe asthma, or balance issues, your doctor might use a chemical stress test instead. You’re given medicine through an IV - like adenosine or dobutamine - that tricks your heart into acting like it’s exercising. You might feel flushed, short of breath, or have a funny taste in your mouth. It’s uncomfortable, but it’s temporary. The test still monitors your ECG and blood pressure, just like the treadmill version.
What’s Better: Stress ECG, Echo, or Nuclear?
Not all stress tests are the same. There are three main types, each with strengths and trade-offs.Standard Exercise ECG is the most common. It’s affordable, widely available, and doesn’t use radiation. But it’s not perfect. Studies show it catches about 68% of coronary artery disease cases - meaning nearly 1 in 3 can be missed, especially in women.
Stress Echocardiography adds ultrasound imaging. Before and after exercise, a technician takes pictures of your heart using a probe on your chest. If a part of the heart muscle doesn’t move as well during stress, it’s likely not getting enough blood. This method is more accurate than a plain ECG - specificity jumps to around 88% - and it has no radiation. It’s especially useful for women, older adults, and people with abnormal resting ECGs.
Nuclear Stress Test uses a small amount of radioactive dye injected into your bloodstream. A special camera then takes pictures of your heart at rest and during stress. Areas with poor blood flow show up as dark spots. This test is the most sensitive - catching about 85% of blockages - but it exposes you to radiation. One test equals about 3-4 years of natural background radiation. It’s usually reserved for higher-risk patients or when other tests are unclear.
Costs vary. A nuclear test can run nearly $1,000, while a stress echo is around $500, and a standard ECG stress test is often under $400. Insurance usually covers them if they’re medically necessary, but out-of-pocket costs depend on your plan.
Who Gets Tested - and Who Doesn’t
Doctors don’t order these tests for everyone. Guidelines say they’re most useful for people with intermediate risk - meaning you have some symptoms (like chest discomfort with activity) and some risk factors (like high blood pressure, smoking, or diabetes), but no clear signs of heart disease yet.For low-risk people - say, a healthy 40-year-old with no symptoms - stress tests often cause more harm than good. They can lead to false positives, which trigger more tests, more anxiety, and even unnecessary procedures.
For high-risk people - someone who just had a heart attack or has severe chest pain at rest - doctors skip stress tests entirely. They go straight to more advanced imaging or emergency care.
There’s also a big blind spot: women. Studies show ECG stress tests miss heart problems in women more often than in men. Why? Women’s heart disease often affects smaller arteries (microvascular disease), which don’t show up on standard tests. That’s why stress echocardiography is now recommended for middle-aged women with symptoms. It picks up problems that ECGs miss.
What to Expect Before, During, and After
Preparing for a stress test is simple, but you can’t skip the details.- 24 hours before: Avoid caffeine - coffee, tea, soda, chocolate, even some painkillers. Caffeine can interfere with the drugs used in chemical stress tests.
- On the day: Wear loose, comfortable clothes and walking shoes. No lotions or oils on your chest - they mess with the electrode sticks.
- During the test: You’ll be monitored closely. Tell the technician immediately if you feel dizzy, short of breath, or have chest pain. The test stops if you do.
- After the test: You can usually drive home and go back to normal activities. Results aren’t always instant, but many clinics give you a quick summary before you leave.
Side effects are rare but possible. In chemical stress tests, about 15% of people feel flushing, nausea, or chest pressure. These pass quickly. In exercise tests, 22% report muscle fatigue or discomfort - normal for pushing your body. Anxiety is common too. One in three patients worry about results before the test even starts. That’s normal. But remember: these tests are designed to protect you.
What Happens If the Test Is Abnormal?
An abnormal result doesn’t mean you need surgery. It means your doctor needs to dig deeper. Often, the next step is a coronary CT angiogram - a scan that shows the actual arteries. Or, if you’re at high risk, a cardiac catheterization might be recommended.Some people get inconclusive results. That happens in about 25% of intermediate-risk cases. It doesn’t mean something’s wrong - just that the test didn’t give a clear answer. Your doctor might suggest a different type of stress test, or wait and monitor you over time.
On the flip side, a normal stress test is reassuring. But it’s not a free pass. Heart disease can still develop. Staying active, eating well, and managing blood pressure and cholesterol matter more than ever.
What’s New in Heart Testing
Technology is changing how we test hearts. Artificial intelligence is now helping doctors interpret ECGs faster and more accurately - improving detection rates by up to 22%. Portable devices like the Cardiac Dynamics StressPal are being used in clinics, nursing homes, and even pharmacies, making stress testing more accessible.Researchers are also getting better at spotting microvascular disease - the kind that affects tiny heart arteries, especially in women. By combining stress echocardiography with advanced imaging techniques like speckle-tracking, doctors can now detect problems in 89% of cases where traditional tests failed.
And radiation? It’s dropping. Since 2021, new FDA guidelines have pushed clinics to cut radiation doses in nuclear tests by 35%. That means safer testing without losing accuracy.
Final Thoughts
ECGs and stress tests aren’t scary. They’re tools - simple, safe, and surprisingly powerful. They don’t replace a healthy lifestyle, but they give you and your doctor a real-time look at how your heart is holding up. Whether you’re worried about chest pain, have a family history, or just want peace of mind, these tests can make all the difference.If your doctor recommends one, ask: Why this test? What are we looking for? What happens next? Understanding the why behind the test takes the guesswork out - and puts you back in control.

Anu radha
December 17 2025I got my stress test last year and was scared to death. But it was so simple, just walking on a machine. No needles, no pain. My heart was fine. Thank you for explaining it so clearly.