When you're taking digoxin for heart failure or atrial fibrillation, even small changes in your diet, other medications, or health status can push you into dangerous territory. This isn't just a theoretical risk - it's a real, life-threatening one. Digoxin has a very narrow window between helping your heart and harming it. Too little, and it doesn't work. Too much, and you could end up in the ER with nausea, blurry vision, or even a dangerous heart rhythm. The good news? Most of these risks are preventable - if you know what to watch for.
Why Digoxin Is Tricky to Manage
Digoxin, sold under brand names like Lanoxin and Crystodigin, works by making your heart beat stronger and more regularly. It's been around since the 1930s, derived from the foxglove plant. But unlike newer heart medications, digoxin doesn't just work - it's finicky. Its therapeutic range is tiny: 0.5 to 0.9 ng/mL in your blood. Anything above 2.0 ng/mL is toxic. And here's the kicker: you can hit that toxic level even if your dose hasn't changed. Why? Because digoxin interacts with so many other things you take - or eat - every day.
According to the American Heart Association, about 12% of heart failure patients in the U.S. still use digoxin. That’s over 700,000 people. And among those over 80, the number jumps to 22%. Why? Because it’s cheap - about $4 to $6 a month for the generic - and it still helps some people who haven’t responded to other treatments. But cost doesn’t mean safety. The risk of toxicity is real. Studies show 0.8% to 4% of people on steady digoxin doses still develop toxicity. And for older adults with kidney issues? That risk soars.
Top 5 Drug Interactions That Can Turn Digoxin Dangerous
Some medications don’t just mix poorly with digoxin - they make it more toxic. Here are the biggest offenders:
- Dronedarone (Multaq): Used for atrial fibrillation, this drug can spike digoxin levels by over 50%. The 2012 PALLAS trial found patients on both had a 2.5-fold higher risk of sudden death. If you're prescribed dronedarone, your digoxin dose must be cut in half - and your blood levels checked weekly.
- Verapamil and Diltiazem (Calan, Cardizem): These calcium channel blockers slow your heart rate and reduce how fast your kidneys clear digoxin. Together, they can cause heart rates below 40 bpm. In the 2019 BEAUTIFUL trial substudy, 18% of patients on digoxin and ivabradine dropped below 35 bpm - enough to need a pacemaker.
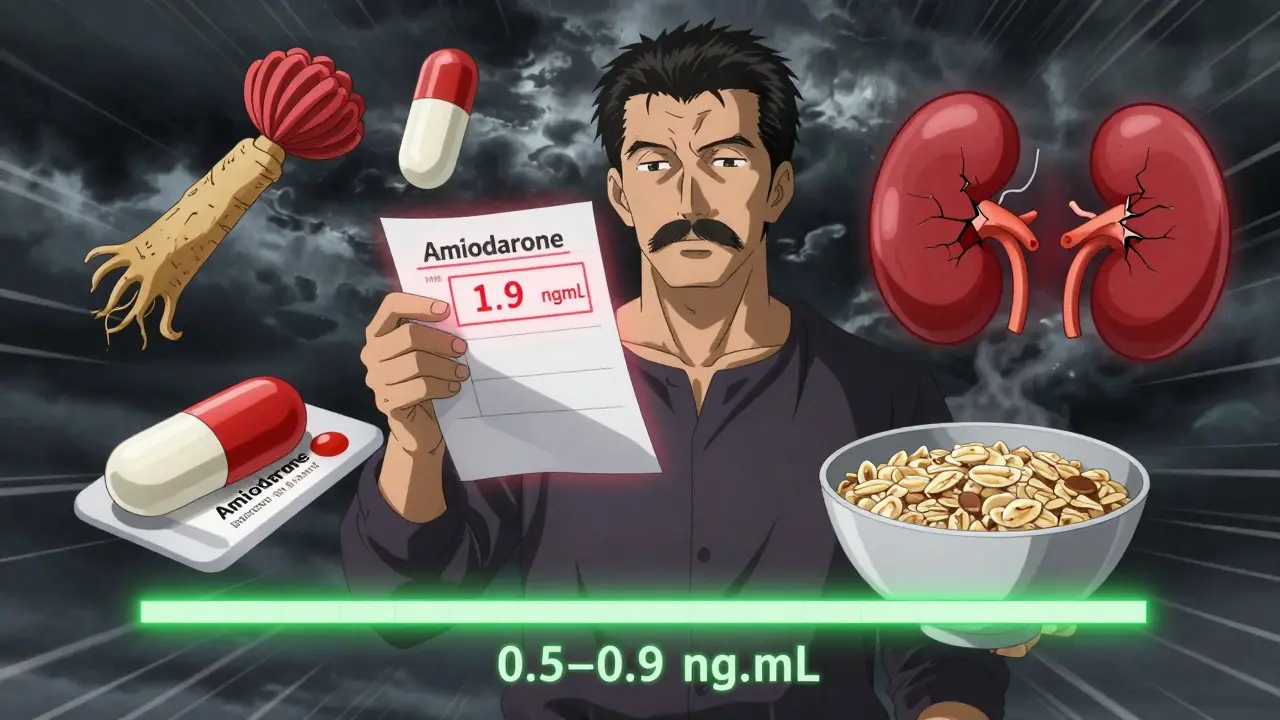
- Amiodarone (Cordarone): A powerful antiarrhythmic, amiodarone can raise digoxin levels by 100% or more. One patient on Reddit reported his levels jumped from 0.8 to 1.9 ng/mL within two weeks - leading to nausea and vision changes. His dose had to be cut by half.
- Quinidine: This older antiarrhythmic can increase digoxin levels by up to 100% by blocking its kidney clearance. Even if you’ve been stable for years, adding quinidine can push you into toxicity.
- Rifampin: Used for tuberculosis, this antibiotic speeds up how your body breaks down digoxin - dropping levels below therapeutic range. You might think your medication isn’t working, when really, it’s being flushed out too fast.
These aren’t rare cases. The Heart Failure Society of America found that 37% of patients had at least one digoxin-related adverse event in their first six months - and most were tied to drug interactions.
What You Eat (and Don’t Eat) Matters More Than You Think
Digoxin doesn’t just interact with pills - it reacts to food and supplements too.
- Black licorice: Yes, really. The glycyrrhizin in licorice lowers potassium levels. Low potassium + digoxin = high risk of fatal arrhythmias. The Heart and Stroke Foundation of Canada warns patients to avoid it entirely.
- Oatmeal, high-fiber cereals, and psyllium supplements: These bind to digoxin in your gut and block absorption. A 2018 study showed oatmeal reduces digoxin levels by 20-25%. One patient on Reddit switched from taking digoxin with breakfast to taking it two hours before - and his levels stabilized.
- Antacids with aluminum or magnesium: These can cut digoxin absorption by up to 30%. Mayo Clinic data shows 22% of digoxin-related ER visits were due to OTC antacids.
- St. John’s wort: This herbal supplement for depression boosts a liver enzyme that clears digoxin faster. Studies show it can drop digoxin levels by 25% - making your medication ineffective.
- Hawthorn: Often marketed for heart health, hawthorn can prolong the QT interval. Combined with digoxin, it raises the risk of torsades de pointes - a dangerous, potentially fatal rhythm.
If you’re taking supplements, tell your doctor. Many patients don’t think of them as “medications,” but they can be just as risky as prescriptions.
Electrolytes: The Silent Trigger
Your potassium level is one of the most important numbers to track when you’re on digoxin. Low potassium - hypokalemia - makes your heart extra sensitive to digoxin’s effects. Even a level below 3.5 mmol/L can trigger toxicity, even if your digoxin dose is perfectly in range.
Diuretics like furosemide (Lasix) and hydrochlorothiazide are common in heart failure patients - but they drain potassium. Corticosteroids do the same. So if you’re on digoxin and a diuretic, your potassium needs checking at least once a month. Some patients get their levels checked every two weeks when starting a new diuretic.
Don’t just rely on your doctor. Learn the signs of low potassium: muscle weakness, cramps, constipation, or heart palpitations. If you feel off, get tested - don’t wait for your next appointment.
Who’s at Highest Risk?
Digoxin isn’t equally risky for everyone. Certain factors make toxicity far more likely:
- Age over 75: Your kidneys clear digoxin slower. Patients over 75 are 2.8 times more likely to have toxicity.
- Low body weight (under 60 kg): Smaller bodies need lower doses. A standard 0.125 mg dose can be too much for someone small.
- Impaired kidney function: If your creatinine clearance is below 50 mL/min, your risk jumps. The FDA and EMA now restrict digoxin use in patients with severe kidney disease (clearance under 15 mL/min).
- Pre-existing heart block or sinus node disease: Digoxin can worsen slow heart rhythms. One 2017 meta-analysis found a 4.3-fold higher risk of fatal heart block in these patients.
The American College of Cardiology now uses a simple risk score to help doctors decide who needs tighter monitoring. Points are given for age over 75, low potassium, high creatinine, high digoxin dose, and use of drugs like verapamil or amiodarone. A score of 5 or more means weekly blood tests are needed - not every six months.
What You Should Do Right Now
If you’re on digoxin, here’s your action plan:
- Know your blood level. Ask your doctor for your last digoxin level. If you don’t know it, request a test. The ideal range is 0.5-0.9 ng/mL.
- Check your potassium. Make sure it’s above 4.0 mmol/L. If it’s below 3.5, talk to your doctor about adjusting your diuretic or adding a potassium supplement.
- Review every medication. This includes OTC drugs, supplements, and herbal products. Bring a list to every appointment.
- Take digoxin on an empty stomach. Wait at least two hours after eating - especially if your breakfast includes oatmeal, fiber bars, or bran.
- Avoid black licorice. Not just candy - check labels on teas, candies, and chewing tobacco.
- Watch for warning signs. Nausea, vomiting, diarrhea, blurred vision, yellow-green halos around lights, or a slow heartbeat (under 50 bpm) are red flags. Don’t wait - call your doctor.
Many patients don’t realize how much control they have. You’re not just passively taking a pill - you’re managing a delicate balance. Small changes in your routine can make a big difference.
What’s Changing in Digoxin Care?
Digoxin use has dropped by 38% since 2010 - not because it’s useless, but because safer options exist. Still, it’s not going away. New research is making it safer. The DIG-FAST trial is testing an extended-release version that reduces blood level spikes by 30%. Early results suggest fewer interactions and less toxicity.
Point-of-care digoxin testing - a quick finger-prick test in the clinic - is now recommended by the European Society of Cardiology. A 2021 JACC study showed it cut toxicity events by 27% compared to waiting for lab results.
And while newer drugs like SGLT2 inhibitors and ARNIs have taken center stage in heart failure, digoxin still has a role - especially for patients with persistent symptoms, atrial fibrillation, or limited financial resources. The key isn’t avoiding it - it’s managing it smartly.
Can I take digoxin with my morning oatmeal?
No. High-fiber foods like oatmeal, bran, and psyllium supplements can reduce digoxin absorption by 20-40%. Take digoxin at least two hours before eating breakfast to ensure full absorption. Many patients who switched to this timing saw their blood levels stabilize within weeks.
Is digoxin safe if I have kidney problems?
It depends. If your kidney function is mild to moderate (creatinine clearance above 30 mL/min), digoxin can still be used - but at a lower dose and with closer monitoring. If your clearance is below 15 mL/min, most guidelines now advise against using digoxin due to high toxicity risk. Always get your kidney function tested before starting or continuing digoxin.
What should I do if I miss a dose of digoxin?
If you miss a dose and remember within 12 hours, take it as soon as you can. If it’s been more than 12 hours, skip the missed dose and take your next one at the regular time. Never double up. Digoxin builds up slowly in your body - skipping one dose won’t hurt, but doubling up could push you into toxicity.
Can I drink alcohol while taking digoxin?
Moderate alcohol (one drink per day) is usually okay, but heavy drinking can worsen heart rhythm problems and lower potassium levels - both of which increase digoxin toxicity risk. If you have atrial fibrillation, alcohol can trigger episodes. Talk to your doctor about what’s safe for you.
How often should I get my digoxin levels checked?
If you’re stable and not on interacting drugs, every 3-6 months is typical. But if you start a new medication, change your dose, or develop kidney issues, get tested weekly for the first 2-4 weeks. The American College of Cardiology recommends weekly testing during any change in therapy.
Are there any signs of digoxin toxicity I can watch for at home?
Yes. Early signs include nausea, vomiting, loss of appetite, and diarrhea. Later signs are more serious: blurry or yellow-green vision, seeing halos around lights, confusion, or a heart rate below 50 bpm. If you notice any of these, stop taking digoxin and call your doctor immediately. Don’t wait.
Why does my doctor keep asking about my potassium?
Low potassium makes digoxin much more toxic - even if your digoxin level is normal. Diuretics, steroids, and even some laxatives can lower potassium. Your doctor checks it because keeping your potassium above 4.0 mmol/L is one of the simplest ways to prevent a dangerous reaction.
Final Thoughts
Digoxin isn’t a drug you can take and forget. It demands attention - to your diet, your other meds, your lab results, and how you feel. But it’s also a tool that still saves lives when used carefully. The goal isn’t to avoid it - it’s to use it wisely. Talk to your doctor, track your numbers, know your limits, and don’t ignore the small things. Because with digoxin, the smallest change can make the biggest difference.

TiM Vince
January 11 2026Digoxin levels are such a nightmare. I’ve been on it for 5 years and my doc only checks it once a year. I didn’t even know oatmeal could mess with absorption until I read this. Now I take it at 7am and eat breakfast at 9am. Small change, huge difference.