What Pharmacists Really Think About Generic Substitution
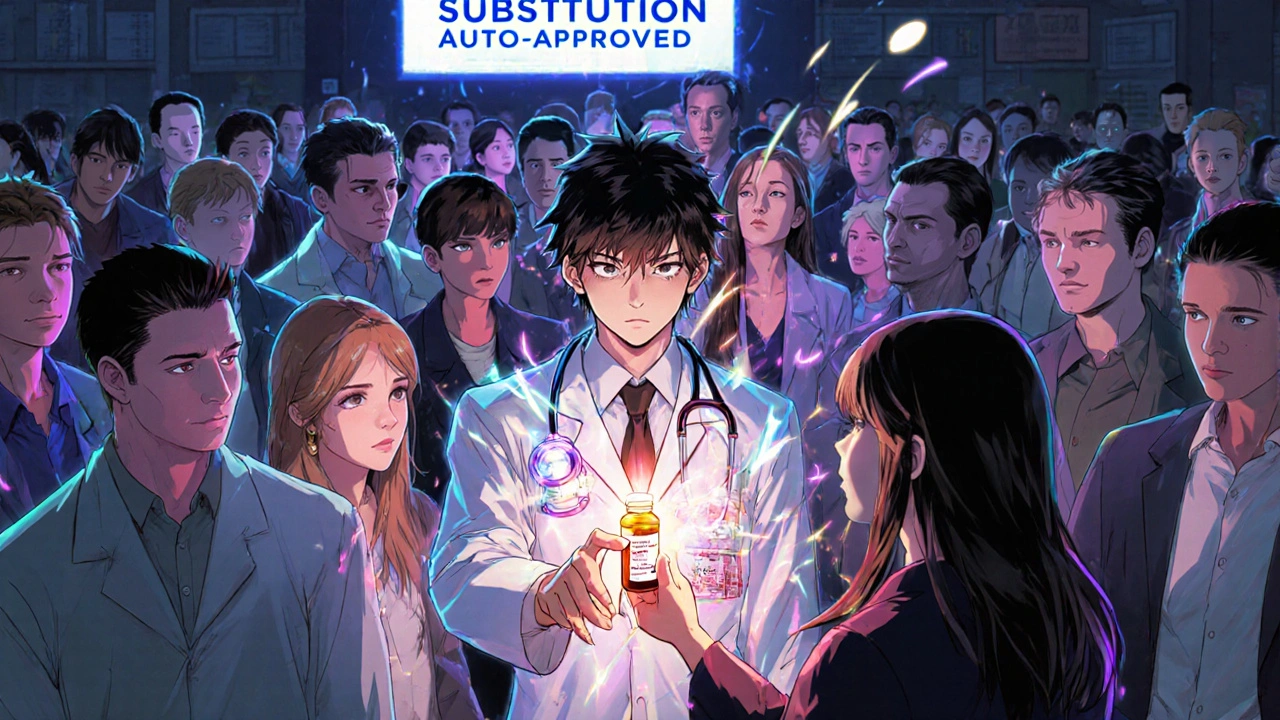
You walk into the pharmacy, hand over your prescription, and get a different-looking pill than what your doctor prescribed. You might not think twice - but the pharmacist? They’re thinking a lot. Generic substitution isn’t just swapping one pill for another. It’s a quiet, high-stakes decision made every day by pharmacists who know the real risks, the patient fears, and the gaps in communication that no one else sees.
The FDA says generics are bioequivalent - meaning they deliver the same active ingredient at the same rate and amount as the brand-name drug. The science checks out: studies show an average difference in absorption of just 3.5% between brand and generic versions. But that number doesn’t tell the whole story. Behind the counter, pharmacists deal with patients who refuse generics because they’re “too cheap,” doctors who hesitate to allow substitutions for epilepsy or thyroid meds, and systems that don’t give them time to explain it all.
Patients Don’t Trust Generics - And Pharmacists Are the Ones Who Have to Fix It
It’s not about price. It’s about perception. A patient might see a white oval pill instead of the blue capsule they’ve taken for years and think, “This isn’t the same.” They’ve heard rumors. They’ve seen commercials that make brand names sound like magic. Some think generics are made in foreign factories with lower standards. Others believe if it costs less, it must be weaker.
Pharmacists hear this every day. In surveys, about one-third of patients report negative experiences after switching to generics - not because the drug failed, but because they felt confused, scared, or misled. Packaging changes. Pill color shifts. Even the shape is different. That’s not a defect. It’s the law. Generic manufacturers can’t copy the exact appearance of brand drugs. But patients don’t know that. And when they notice the change, they assume something went wrong.
One pharmacist in Ohio told me about a 72-year-old woman with high blood pressure who refused her new generic lisinopril because it was “smaller and white.” She’d been on the brand for 12 years. She thought switching meant her condition was getting worse. The pharmacist spent 20 minutes explaining FDA standards, showing her the pill’s active ingredient matched exactly, and even called her doctor to confirm the switch was intentional. She took it - but only because she trusted the pharmacist. Not because she understood it.
Chronic Illness Patients Are the Hardest to Convince
Generics work great for antibiotics, pain relievers, and allergy meds. But for chronic conditions - especially those where tiny changes in blood levels can cause big problems - the stakes are higher. Epilepsy, thyroid disorders, warfarin (a blood thinner), and some antidepressants fall into a category called narrow therapeutic index (NTI) drugs. These meds have a small window between effective and toxic doses. Even a 5% difference in absorption can mean a seizure, a clot, or a relapse.
Doctors know this. Many won’t allow substitution without explicit permission. But pharmacists still get prescriptions for these drugs flagged for automatic substitution by insurance systems. So now they’re stuck: follow the system’s rules and risk patient harm, or override it and risk getting flagged for non-compliance.
Studies show that when patients on anti-epileptic drugs switch generics, up to 15% report increased seizures - though it’s often hard to prove the generic caused it. Still, pharmacists see the pattern. They remember the 19-year-old who went from 2 seizures a month to 12 after switching brands. They remember the woman who stopped taking her thyroid med because she “felt weird” after the pill changed color. They don’t blame the patient. They blame the system that lets substitution happen without clear communication.

Doctors Aren’t Talking About It - So Pharmacists Are Left Holding the Bag
Here’s the truth: most patients don’t know substitution is even an option. A 2015 survey found that 64% of patients never heard from their doctor that a generic could be used. That means when the pharmacist hands them a different pill, they think it’s a mistake - or worse, a cost-cutting trick.
Doctors are busy. They write the script, assume the pharmacy handles it, and move on. But pharmacists are the ones who have to answer the questions: “Why is this cheaper?” “Is this safe?” “Did they give me the wrong medicine?”
And it’s not just patients. Many physicians still believe generics are inferior - even though the FDA has approved over 20,000 generic drugs and found no meaningful difference in effectiveness for the vast majority. One study showed that while 87% of doctors agreed generics save money, only 70% thought they were clinically appropriate. That gap? It’s a chasm. And pharmacists are the ones bridging it.
Time Is the Biggest Enemy
Pharmacists aren’t just dispensing pills. They’re counselors, educators, translators, and sometimes therapists. A typical pharmacy visit lasts less than 5 minutes. But explaining why a generic is safe - especially to someone with dementia, depression, or multiple chronic conditions - takes time.
Australian pharmacists reported that counseling resistant patients - especially those on five or more medications - could add 10 to 15 extra minutes per prescription. That’s not feasible in a busy pharmacy where 200 prescriptions come through in a day. And yet, skipping the explanation risks non-adherence. Patients forget to take their meds because they don’t recognize the pill. Or they stop taking them because they’re afraid. Either way, the hospital readmission rate goes up - and the cost savings from generics vanish.
Worse, only 38% of patients are even told they can refuse a generic substitution. That’s not just poor practice - it’s a violation of patient rights in many states. But most pharmacies don’t have the staffing to ask every patient if they want to opt out. So the system defaults to substitution - and patients are left in the dark.
What Pharmacists Wish They Could Change
Pharmacists aren’t against generics. In fact, 96% of them recommend them when appropriate. But they want a better system. Here’s what they wish would change:
- Doctors should talk to patients first. If the prescriber says, “We’re switching to a generic to save you money and it’s just as safe,” patients are far more likely to accept it.
- Clear labeling on generics. If the pill looked the same, or if the packaging clearly showed “FDA-approved generic equivalent,” patients wouldn’t panic.
- More time for counseling. Pharmacies need dedicated staff or technology to handle patient education without slowing down the entire workflow.
- Exceptions for NTI drugs. Automatic substitution shouldn’t happen for epilepsy, warfarin, or thyroid meds unless the prescriber specifically allows it.
- Transparency about manufacturer changes. If the generic switches from one company to another, patients should be warned. Different manufacturers can have slight differences in fillers or release rates - and that matters for some people.
The Bottom Line: Generics Work - But Only If People Understand Them
Generic drugs save the U.S. healthcare system over $300 billion a year. They’re safe, effective, and regulated by the same standards as brand-name drugs. For most people, switching makes no difference at all.
But for the ones who do feel the change - the elderly, the chronically ill, the anxious, the confused - that small difference in pill shape or color can break trust. And once trust is broken, adherence drops. Costs go up. Health gets worse.
Pharmacists aren’t trying to push generics. They’re trying to protect patients from the confusion created by a system that assumes everyone understands the rules. The solution isn’t to stop substitution. It’s to start communication - early, clearly, and with respect for the patient’s fear, not just the pharmacy’s bottom line.
Are generic drugs really as good as brand-name drugs?
Yes, for the vast majority of medications. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also be bioequivalent - meaning they deliver the drug into the bloodstream at the same rate and amount. Studies show an average absorption difference of just 3.5% between brand and generic versions. For conditions like high blood pressure, diabetes, and infections, generics work just as well.
Why do generic pills look different from brand-name ones?
U.S. law prohibits generic manufacturers from copying the exact appearance of brand-name drugs, including color, shape, and markings. This is to avoid trademark infringement. But the active ingredient is identical. The differences are only in inactive ingredients like dyes or fillers, which don’t affect how the drug works. Still, patients often mistake these changes for a different or weaker medication - which is why pharmacists need to explain it.
Can switching to a generic cause side effects or make my condition worse?
For most drugs, no. But for medications with a narrow therapeutic index - like seizure drugs (e.g., phenytoin), thyroid meds (levothyroxine), or blood thinners (warfarin) - even small changes in absorption can matter. Some patients report changes in symptoms after switching, though studies can’t always prove the generic caused it. Pharmacists are trained to flag these cases and often recommend staying on the same version unless the doctor approves a switch.
Can I refuse a generic substitution?
Yes. In most states, you have the legal right to ask for the brand-name drug instead, even if a generic is available. However, you may have to pay more out of pocket. Pharmacists are required to inform you of this option - but many don’t, because they’re rushed. If you want the brand, say so clearly when you pick up your prescription.
Why do pharmacists recommend generics so often?
Because they’re proven safe, effective, and save patients an average of 21% on medication costs. Pharmacists see how many people skip doses because they can’t afford their prescriptions. By recommending generics, they’re helping patients stay on their meds - which prevents hospital visits and long-term health problems. Most pharmacists recommend generics in 96% of eligible cases because they want their patients to get the treatment they need - without financial stress.
Do pharmacists get paid more for dispensing generics?
Not usually. Most pharmacies make the same profit margin on brand and generic drugs. Pharmacists aren’t pushing generics to make more money - they’re pushing them because they know it helps patients afford their treatment. The real financial incentive comes from insurance companies, which often require generics unless the doctor specifically writes “dispense as written” or “no substitution.”


Jessica Healey
November 17 2025My grandma switched to generic levothyroxine and started feeling like a zombie. She didn’t say anything till she collapsed at church. Turns out the filler in the new pill made her stomach reject it. Pharmacist had to call her doctor, switch her back, and explain why the ‘same’ pill wasn’t. No one warned her. No one asked. Just another number on a screen.