Most people don’t feel anything when their kidneys start to fail. No sharp pain. No sudden warning. Just quiet, slow damage that slips past routine checkups - until it’s too late. Chronic kidney disease (CKD) affects 37 million Americans, and 90% of them don’t even know they have it. That’s not because they’re ignoring their health. It’s because the early signs are invisible. By the time fatigue, swelling, or nausea show up, the kidneys are already severely damaged. But here’s the truth: if you catch CKD early, you can slow or even stop it. And the key isn’t waiting for symptoms. It’s understanding the stages - and knowing what tests actually matter.
What Chronic Kidney Disease Really Means
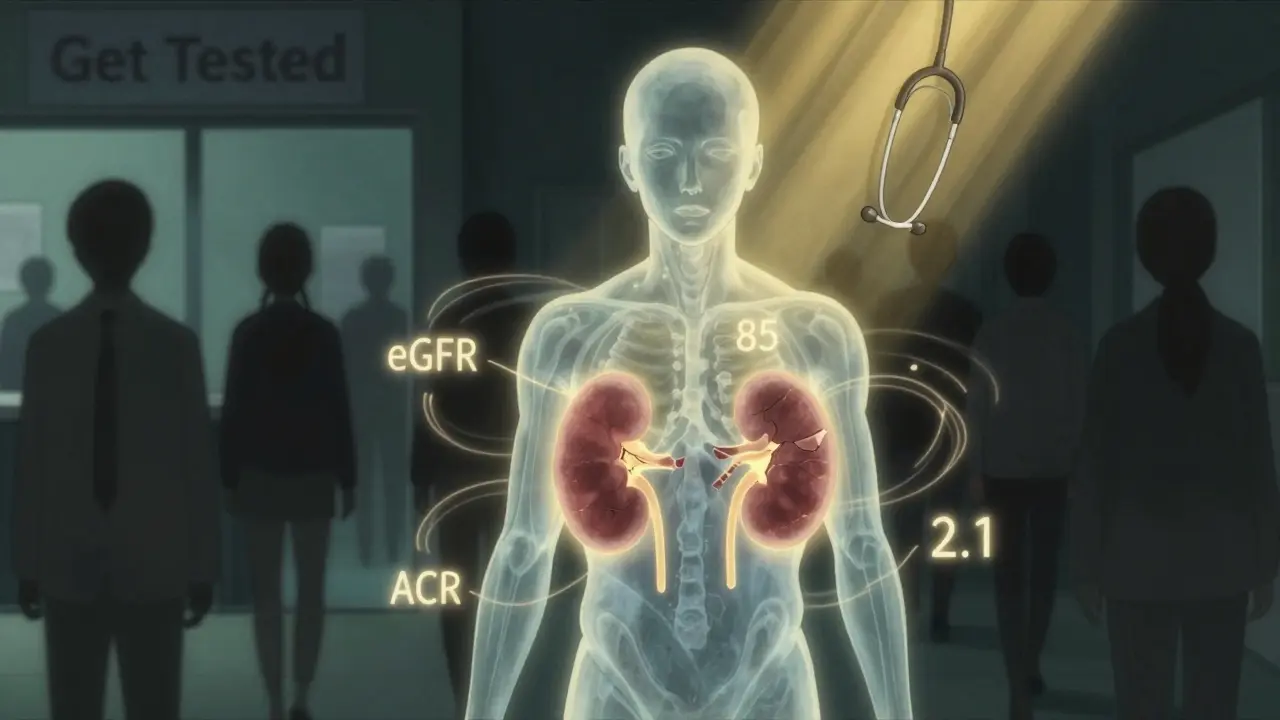
Chronic kidney disease isn’t a single event. It’s a long-term decline in how well your kidneys filter waste and balance fluids. The kidneys don’t just make urine. They regulate blood pressure, produce red blood cell hormones, and keep your bones strong. When they’re damaged over three months or more - that’s CKD. It doesn’t mean you’re about to need dialysis. It means your kidneys are working less efficiently than they should, and that decline can be tracked, managed, and sometimes reversed - if you act in time.The current standard, set by Kidney Disease: Improving Global Outcomes (KDIGO), uses two main numbers to define CKD: your eGFR and your albuminuria level. eGFR tells you how well your kidneys are filtering blood. Albuminuria measures protein leaking into your urine - a sign your kidney filters are broken. Together, they give a complete picture. Neither one alone is enough.
The Six Stages of CKD: What Your Numbers Really Mean
Your eGFR is calculated from a simple blood test that measures creatinine. But not all eGFRs are created equal. The 2021 CKD-EPI equation, now the gold standard, removed race-based adjustments after studies showed they led to underdiagnosis in Black patients. Here’s what your numbers mean:- Stage G1 (eGFR ≥90): Your kidneys are filtering normally, but there’s damage. This could mean protein in your urine, abnormal imaging, or a history of kidney disease. You might feel fine - but you’re not risk-free.
- Stage G2 (eGFR 60-89): Mild reduction. Kidney function is still close to normal, but persistent protein leakage or structural changes confirm CKD. Many people here are diagnosed by accident - during a routine blood test for high blood pressure or diabetes.
- Stage G3a (eGFR 45-59): Mild to moderate loss. This is where things start to shift. Your risk of heart disease jumps. If you also have moderate to high albuminuria, your chance of progressing to kidney failure within five years doubles.
- Stage G3b (eGFR 30-44): Moderate to severe loss. At this point, specialists recommend regular nephrology visits. Many patients here still don’t feel symptoms, but their kidneys are losing ground fast.
- Stage G4 (eGFR 15-29): Severe loss. Your kidneys are working at less than 30% capacity. You’ll likely need to plan for dialysis or transplant. Diet changes, blood pressure control, and avoiding kidney-toxic medications become critical.
- Stage G5 (eGFR <15 or on dialysis): Kidney failure. At this stage, your body can’t clean itself. Dialysis or a transplant is the only way to survive. About 98% of people here will need one or the other.
Albuminuria adds another layer. It’s measured as ACR - albumin-to-creatinine ratio in urine. A1 means less than 3 mg/mmol (normal), A2 is 3-30 (moderate), and A3 is over 30 (severe). A person with Stage G3a and A3 albuminuria has a 5.4 times higher risk of dying than someone with the same eGFR but normal urine protein. That’s why both numbers matter.
How Fast Does CKD Progress? It Depends on You
Not everyone with CKD heads to dialysis. In fact, most don’t. Progression speed varies wildly. Someone with Stage G3a and A1 albuminuria might never progress. Someone with G3b and A3 could reach kidney failure in under five years. The biggest drivers of progression? Uncontrolled diabetes, high blood pressure, smoking, obesity, and certain medications like NSAIDs (ibuprofen, naproxen). A 2018 SPRINT trial showed that using ACE inhibitors or ARBs in patients with proteinuria and Stage G3a reduced progression to Stage G4 by 37%. That’s not a small win. That’s life-changing.But here’s the catch: many people don’t know they have protein in their urine. Routine blood tests don’t catch it. You need a specific urine test - the ACR test. And it has to be done right: a first-morning sample, not a random one. Two abnormal results, at least 90 days apart, are needed to confirm CKD. One bad test? Could be dehydration, infection, or exercise. Two? That’s a signal.

Why Most People Get Diagnosed Too Late
The National Kidney Foundation’s 2022 patient survey found that 78% of people diagnosed with Stage G2 or G3 had no symptoms. They didn’t feel tired. Their legs didn’t swell. They weren’t nauseous. Their diagnosis came from a blood test done for something else - a knee surgery check, a diabetes screen, or a routine physical. That’s the problem. CKD is silent until it’s advanced.One Reddit user, ‘DialysisDad,’ shared his story: he had diabetes for years but never got his urine tested. When he finally felt weak and puffy, his eGFR was 19 - Stage G4. His doctor said he should have been monitored years earlier. He wasn’t. That delay cost him time, options, and peace of mind.
On the flip side, patients diagnosed early - at Stage G2 or G3 - report 32% higher adherence to treatment and 41% more confidence managing their condition. They had time to learn, adjust, and plan. They weren’t thrown into crisis.
Who Should Be Tested - And When
You don’t need to wait for symptoms. If you have any of these, get tested every year:- Diabetes (type 1 or 2)
- High blood pressure
- Heart disease
- Family history of kidney failure
- Obesity (BMI over 30)
- Age over 60
- Being Black, Native American, or Hispanic (higher risk groups)
The test is simple: a blood draw for creatinine (to calculate eGFR) and a urine dipstick or lab test for ACR. No fasting. No special prep. Just a morning sample. If you’re over 50 and have one risk factor, ask your doctor. Don’t wait for them to bring it up.
The New Tools Making Early Detection Possible
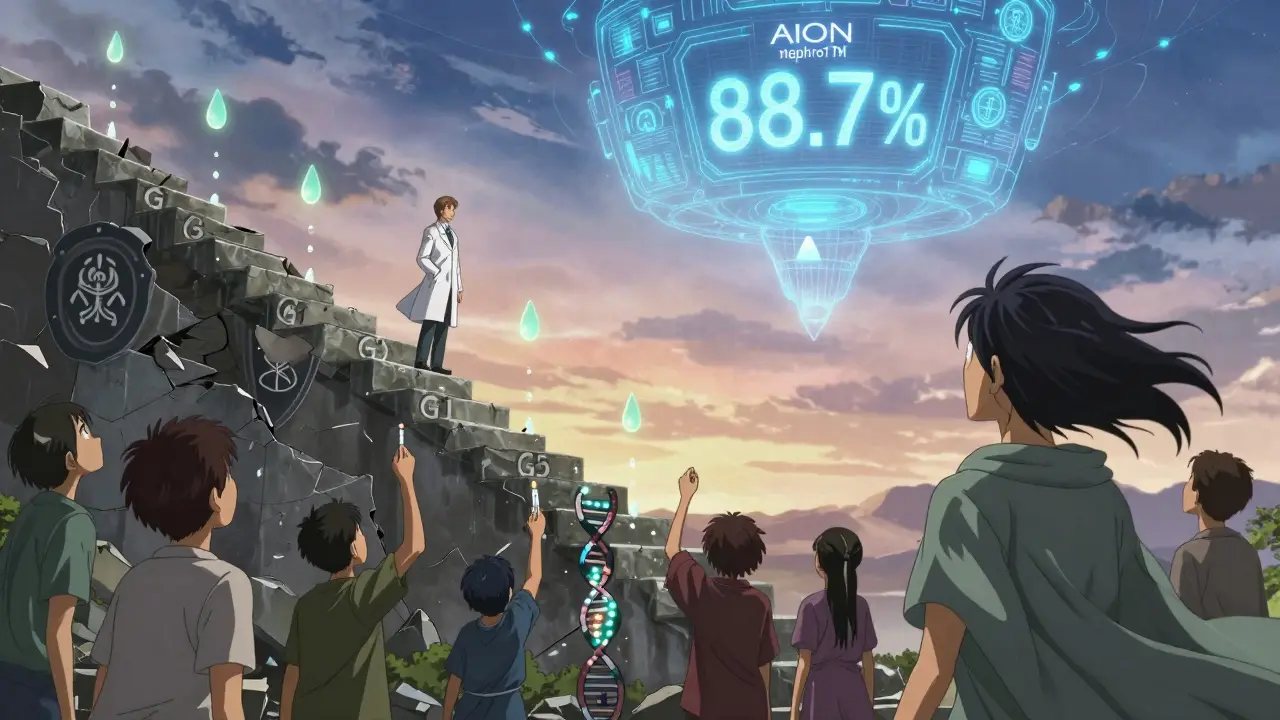
Technology is catching up. In 2023, the FDA approved the first AI-based tool - AION nephroTM - that analyzes 27 clinical factors to predict your risk of eGFR decline over two years with 88.7% accuracy. It’s not in every clinic yet, but it’s coming. Point-of-care eGFR devices are cutting lab wait times from days to minutes. Mobile screening units in places like Baltimore have already found over 1,200 undiagnosed cases in just one year.Soon, genetic risk scores may help too. A 2023 study identified 17 gene variants that predict how fast CKD will progress in an individual. Within five years, your kidney risk might be measured not just by your numbers - but by your DNA.
What Happens If You’re Diagnosed Early?
If you’re in Stage G1 or G2, your doctor will likely focus on controlling your blood pressure and blood sugar, stopping smoking, and avoiding NSAIDs. You might be prescribed an ACE inhibitor or ARB - even if your blood pressure is normal - because they protect your kidneys directly. You’ll get your eGFR and ACR checked every 6-12 months. That’s it. No dialysis. No drastic changes. Just smart, consistent care.At Stage G3, you’ll probably see a nephrologist. Diet changes become more important: less salt, controlled protein intake, avoiding processed foods. You’ll be monitored for anemia, bone disease, and fluid buildup. But you’re still not on dialysis. You’re still in control.
Early diagnosis doesn’t mean a life sentence. It means a head start. It means you get to choose your path - not have it forced on you.
The Psychological Cost of a CKD Label
There’s a dark side to early detection. Some people - especially those with Stage G2 and normal albuminuria - feel terrified after getting the label. They imagine dialysis, death, and isolation. A 2021 UK study found 22% of early-stage patients experienced what they called ‘diagnostic distress’ - anxiety from being told they have a chronic disease, even when their kidneys are barely affected.This is why how you’re told matters. Doctors need to explain: ‘You have early kidney changes, but we can manage this. You’re not broken. You’re not doomed.’ The goal isn’t to scare you. It’s to empower you.
Some experts even argue that Stage G3a should be called ‘mildly reduced kidney function’ - not CKD - to avoid unnecessary panic. That debate is still ongoing. But one thing’s clear: labeling without context hurts. Knowledge without fear helps.
What You Can Do Today
You don’t need to wait for your next physical. If you’re at risk, take action now:- Ask your doctor for an eGFR and ACR test - even if you feel fine.
- If you have diabetes or high blood pressure, get tested every year - no exceptions.
- Stop taking ibuprofen or naproxen regularly unless your doctor says it’s safe.
- Reduce salt. Avoid processed snacks, canned soups, and fast food.
- Keep your blood pressure under 130/80. Keep your HbA1c under 7% if you’re diabetic.
- Don’t smoke. It’s one of the fastest ways to wreck your kidneys.
CKD isn’t a death sentence. It’s a warning. And warnings are meant to be heeded - not ignored.
Can you reverse chronic kidney disease?
You can’t fully reverse damage that’s already happened, but you can stop or slow further decline - especially in Stages G1-G3. Controlling blood pressure, managing diabetes, avoiding NSAIDs, and using kidney-protective medications like ACE inhibitors can preserve remaining function. Some people with early-stage CKD stabilize for decades without progression.
Is a low eGFR always a sign of kidney disease?
Not always. About 40% of adults over 70 have an eGFR below 60 due to normal aging, not disease. That’s why doctors look at both eGFR and albuminuria. If your urine is clean and your eGFR is stable, you likely don’t have progressive CKD. But if protein is leaking or your eGFR is dropping fast, that’s a red flag.
What’s the difference between eGFR and creatinine?
Creatinine is a waste product your muscles make. Your blood test shows how much is in your blood. eGFR is a calculated number - it uses your creatinine level, age, sex, and race (no longer) to estimate how well your kidneys are filtering. It’s the real measure of kidney function. One tells you what’s in your blood. The other tells you how well your kidneys are working.
Can I check my kidney health at home?
You can’t measure eGFR at home - you need a blood test. But some home urine strips can detect protein, though they’re not as accurate as lab ACR tests. If a home test shows protein, see your doctor for a proper ACR test. Don’t rely on strips alone. They’re a flag, not a diagnosis.
Does drinking more water help my kidneys?
Drinking water doesn’t improve kidney function if you already have CKD. But staying hydrated helps your kidneys work efficiently and prevents kidney stones. Don’t overdo it - too much water can be dangerous, especially if you’re on dialysis or have heart issues. Drink when you’re thirsty. Don’t force gallons.
Are there foods I should avoid with CKD?
Yes - especially if you’re in Stage G3 or later. Limit salt, processed meats, canned foods, soda, and foods high in phosphorus (like colas, processed cheese, and fast food). Too much potassium can also be risky if your kidneys can’t filter it. A renal dietitian can help you adjust your meals safely.
Why do some people with CKD never need dialysis?
Because they caught it early and managed it well. Many people with Stage G1-G3 live full lives without ever reaching kidney failure. The key is controlling the things that make CKD worse - diabetes, high blood pressure, smoking, and NSAIDs. With good management, progression can be halted for decades.

Bret Freeman
December 25 2025This is the kind of information that should be plastered on every doctor's waiting room wall. People think if they don't feel sick, they're fine. That's how you end up on dialysis at 45. The fact that 90% of people with CKD don't know they have it isn't a medical failure-it's a societal one. We celebrate fitness influencers but ignore the quiet killers in our bloodwork.