When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But how does the FDA make sure it really does? The answer lies in bioequivalence - a strict scientific standard that bridges the gap between brand-name drugs and their cheaper copies.
What Bioequivalence Actually Means
Bioequivalence isn’t about matching ingredients by weight. It’s about matching how your body handles the drug. The FDA defines it as the absence of a significant difference in how fast and how much of the active ingredient enters your bloodstream compared to the original brand-name drug. That’s it. No more, no less.Think of it like two identical cars driving the same route. One’s a new model, the other’s a copy. Bioequivalence checks if both cars reach the same speed at the same time, and cover the same total distance - not whether they have the same paint job or radio.
This standard was created under the Hatch-Waxman Act of 1984. Before that, generic manufacturers had to repeat expensive clinical trials just to prove their drug worked. The law changed that. Now, they only need to show bioequivalence. That’s why generics cost 80% less on average - not because they’re weaker, but because they don’t repeat the same research.
How the FDA Tests for Bioequivalence
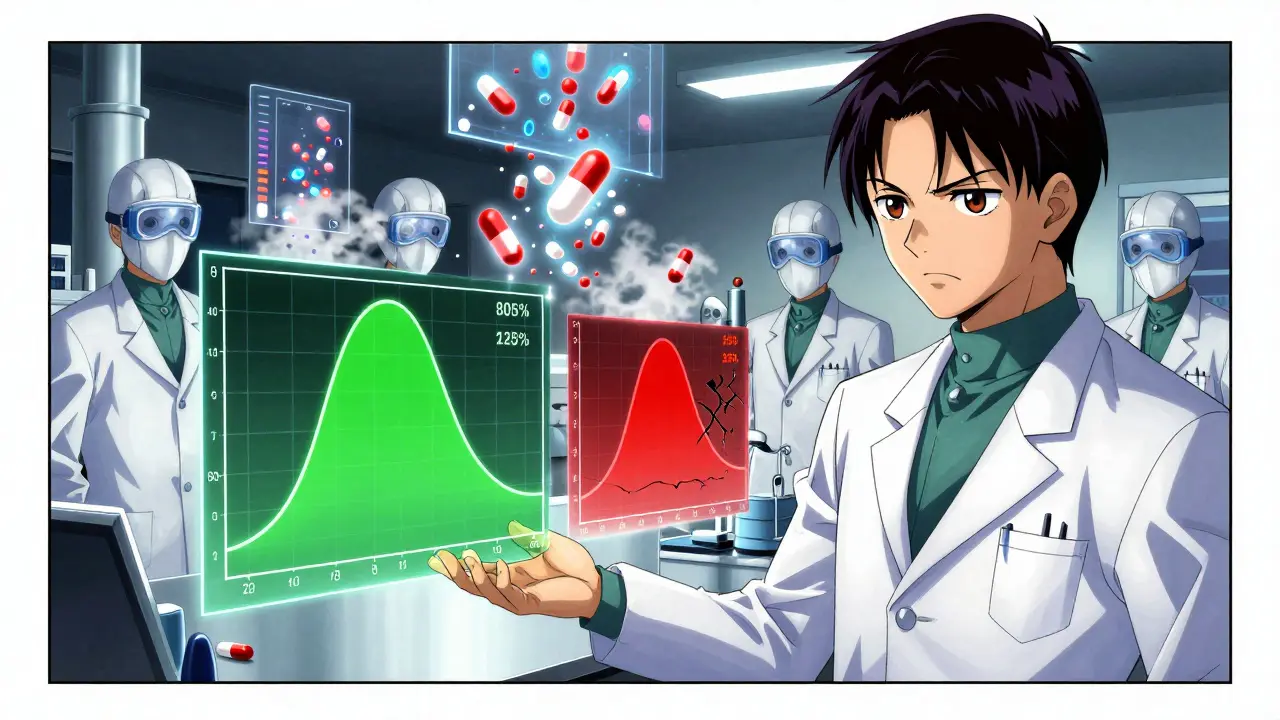
The FDA doesn’t guess. They measure. In controlled studies, 24 to 36 healthy volunteers take both the brand-name drug and the generic version, usually in a random order with a washout period in between. Blood samples are taken over hours - sometimes up to 72 hours - to track how the drug moves through the body.Two key numbers are watched closely:
- Cmax: The highest concentration of the drug in the blood. This tells you how fast it’s absorbed.
- AUC: The total amount of drug absorbed over time. This tells you how much gets into your system.
The FDA requires the ratio of the generic’s average Cmax and AUC to the brand’s to fall between 80% and 125%. But here’s the catch - it’s not just the average. The entire 90% confidence interval must fit inside that range. That means even the lowest possible value (based on the data) can’t dip below 80%, and the highest can’t go above 125%.
For example: If the brand drug’s AUC is 100 units, the generic’s average AUC might be 93. If the 90% confidence interval is 84 to 110, that’s approved. But if the interval stretches to 103 to 130 - even if the average is 116 - it fails. The upper limit is 125%. No exceptions.
Myth: Generic Drugs Can Be 45% Weaker or Stronger
A lot of people think the 80-125% range means the generic can contain anywhere from 80% to 125% of the active ingredient. That’s wrong. The active ingredient amount is tightly controlled. Both versions must contain the same amount, same salt form, same dosage form - that’s called pharmaceutical equivalence.The 80-125% rule applies only to how your body absorbs and uses the drug. Two pills can have exactly 500 mg of the same chemical, but if one dissolves slower in your stomach, the absorption curve changes. That’s what bioequivalence catches.
Studies show this isn’t just theory. In 2022, the FDA reviewed over 1,000 generic applications. About 65% got approved on the first try. The rest failed mostly because of formulation issues - things like coating, fillers, or how fast the pill breaks down - not because the active ingredient was wrong.
When the Rules Get Tighter
For most drugs, the 80-125% range works fine. But for drugs with a narrow therapeutic index - where even small changes can cause side effects or treatment failure - the stakes are higher. Think warfarin, lithium, or certain anti-seizure meds. Even a 10% difference in blood levels can be dangerous.Still, the FDA hasn’t changed the rule for these. Why? Because decades of real-world data show that generics approved under the standard range perform just as safely and effectively. The agency monitors adverse events closely. If a pattern emerged, they’d adjust. So far, they haven’t needed to.
Some complex drugs - like inhalers, topical creams, or injectables - are harder to test. For those, the FDA may allow in vitro testing (lab tests on the drug’s physical properties) instead of human trials. But only if the science supports it. For example, if a cream’s particle size, viscosity, and pH are identical to the brand, and it’s proven to release the drug the same way, human bioequivalence studies might not be needed.
Transparency Is Now the Rule
Until 2021, generic companies only had to submit bioequivalence studies that passed. That meant the FDA never saw the failed attempts. Now, they must submit every single study - successful or not. This change was made to prevent cherry-picking and give regulators a full picture of how a drug behaves.It’s also helping scientists understand why some formulations fail. Was it the manufacturing temperature? The type of binder? The drying time? With more data, the FDA can give better feedback early in development. That’s cutting approval times and reducing costly redesigns.
Why This Matters for You
In 2023, generics made up 90% of all prescriptions filled in the U.S. But they accounted for only about 20% of total drug spending. That’s over $1.7 trillion saved between 2010 and 2019. These savings come from a system that works - because bioequivalence isn’t a loophole. It’s a science-backed guarantee.When your doctor prescribes a generic, you’re not taking a cheaper version. You’re taking the same medicine, proven to behave the same way in your body. The FDA doesn’t approve generics because they’re cheap. They approve them because they’re equivalent.
What’s Next for Bioequivalence
The FDA is now exploring computer modeling and simulation to predict how a drug will behave in the body - without always needing human trials. For some complex generics, this could reduce testing time and cost. But the goal stays the same: ensure safety and effectiveness without unnecessary delays.As new drug forms emerge - like long-acting injectables or oral dissolving tablets - the bioequivalence methods will evolve. But the core principle won’t change: if it doesn’t act the same way in your body, it doesn’t get approved.
Are generic drugs less effective than brand-name drugs?
No. Generic drugs must meet the same strict bioequivalence standards as brand-name drugs. The FDA requires that the rate and extent of absorption into the bloodstream be within 80-125% of the original drug. Decades of real-world use and clinical data confirm that generics perform just as reliably.
Can a generic drug have a different active ingredient?
No. The active ingredient in a generic drug must be identical in chemical structure, strength, and dosage form to the brand-name drug. Differences in inactive ingredients (like fillers or dyes) are allowed, but they cannot affect how the drug works in your body.
Why do some people say generics don’t work as well?
Sometimes, people notice differences in pill size, color, or taste - which are harmless. Other times, switching from one generic to another (both approved) can cause confusion if the formulations differ slightly in release rate. But these are not signs of ineffectiveness. They’re variations in manufacturing, and they’re still within FDA-approved bioequivalence limits.
Does the FDA test every batch of generic drugs?
The FDA doesn’t test every batch, but it inspects manufacturing facilities regularly - often unannounced. They also randomly test drugs on the market. If a batch fails, the FDA can pull it and shut down production until the issue is fixed.
Are bioequivalence studies always done on healthy people?
Yes, for most drugs. Healthy volunteers are used because they provide clean, predictable data without the interference of disease. For drugs that can’t be tested in healthy people - like cancer meds - the FDA may allow studies in patients, but only with special approval and strict safeguards.


Ashley Porter
January 27 2026Let’s be real - the 80-125% range sounds wild until you realize it’s statistically rock solid. The FDA doesn’t wing it. They’ve got confidence intervals tighter than my jeans after Thanksgiving. Cmax and AUC? Yeah, that’s the real MVP duo here. No fluff, just pharmacokinetics.