What Is Audiometry Testing?
Audiometry testing is the standard way doctors measure how well you hear different sounds. It’s not just a simple beep test-it’s a detailed process that maps your hearing sensitivity across frequencies, using decibel levels as the measurement scale. This test helps identify if you have hearing loss, what type it is, and how severe it is. The results are shown on a graph called an audiogram, which looks like a map of your hearing ability.
Every sound you hear travels through your ear in different ways. Audiometry checks both air conduction-how sound moves through your ear canal and eardrum-and bone conduction-how vibrations travel directly through the bones of your skull to the inner ear. By comparing these two, audiologists can tell if the problem is in your outer or middle ear (like wax buildup or an infection) or in your inner ear or auditory nerve (which is often due to aging or noise exposure).
How Decibel Levels Work in Hearing Tests
Decibels (dB) measure loudness, but in hearing tests, they’re not about how loud a sound is in the real world-they’re about how soft you can still hear it. The scale starts at 0 dB HL (hearing level), which is the quietest sound a young person with normal hearing can detect. Anything above 25 dB HL is considered outside the normal range.
Here’s what those numbers mean in real life:
- 0-25 dB HL: Normal hearing-you hear whispers, rustling leaves, and ticking clocks easily.
- 26-40 dB HL: Mild hearing loss-you miss soft speech, especially in noisy rooms.
- 41-55 dB HL: Moderate hearing loss-you struggle with conversations at normal volume.
- 56-70 dB HL: Moderately severe hearing loss-you need people to speak loudly or repeat themselves often.
- 71-90 dB HL: Severe hearing loss-you hear only loud sounds like a vacuum or shouting.
- 91+ dB HL: Profound hearing loss-you may not hear even loud sirens or thunder.
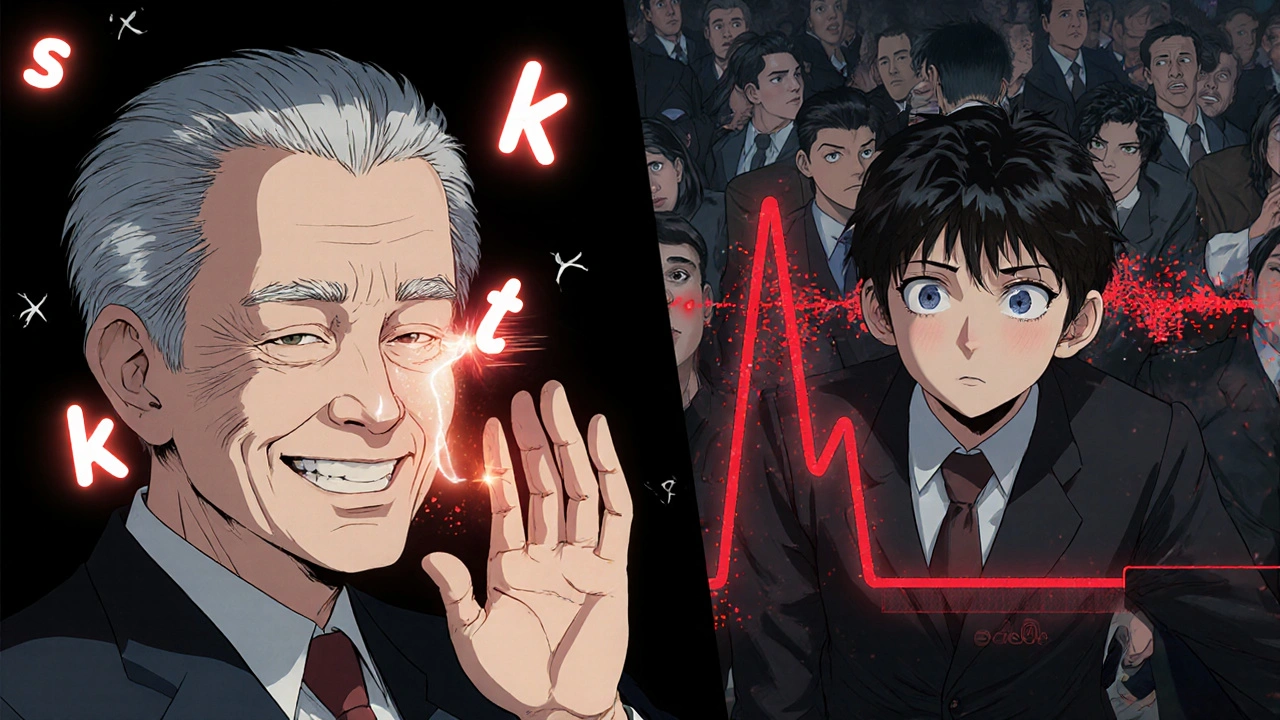
Most people don’t realize how quickly hearing declines. A 60-year-old might have a 45 dB loss at 2,000 Hz-the frequency where consonants like “s,” “t,” and “k” live. That’s why they say, “I can hear you, but I can’t understand what you’re saying.”
The Pure-Tone Audiometry Process
The most common type of hearing test is pure-tone audiometry. You wear headphones, and tones at different pitches (frequencies) play-starting at 1,000 Hz, then 500, 2,000, 4,000, 8,000, 250 Hz. You press a button every time you hear a tone, no matter how faint.
The method used is called the modified Hughson-Westlake technique. It’s not random. The audiologist starts with a tone you can clearly hear, then drops the volume by 10 dB. If you don’t hear it, they raise it by 5 dB until you do. They repeat this until they find the softest level you can detect at least half the time. That’s your threshold.
Testing takes about 10-15 minutes per ear. It’s quiet, non-invasive, and you don’t need to do anything special except stay still and listen. But it’s not foolproof. If you’re tired, distracted, or don’t understand the instructions, your results can be off. That’s why experienced audiologists watch for consistency and use masking-playing noise in the other ear-to make sure you’re not hearing the tone through your other ear.
Bone Conduction and Air-Bone Gaps
After air conduction testing, a small oscillator is placed behind your ear, on the mastoid bone. This sends vibrations straight to your inner ear, skipping your eardrum and middle ear bones. If your bone conduction thresholds are much better than your air conduction ones, you have a conductive hearing loss.
That “gap” between air and bone thresholds is key. If the gap is 15 dB or more at two or more frequencies, it means something is blocking sound in your outer or middle ear. Common causes include earwax, fluid from an infection, or a damaged eardrum. If air and bone thresholds are equally poor, the issue is in your inner ear or nerve-called sensorineural hearing loss. This is often caused by aging, loud noise, or genetics.
People with sudden sensorineural hearing loss need urgent care. If you lose hearing in one ear over a day or two, see a doctor immediately. Steroids can help if given within 72 hours.

Speech Testing: More Than Just Beeps
Beeps tell you how loud you can hear. Speech testing tells you how well you understand. Two key parts: Speech Reception Threshold (SRT) and Word Recognition Score (WRS).
SRT finds the quietest level you can repeat 50% of two-syllable words like “baseball” or “hotdog.” It should match your average pure-tone hearing level at 500, 1,000, and 2,000 Hz-within 10 dB. If it doesn’t, something’s wrong. Maybe you’re not trying, or there’s a neurological issue.
WRS is harder. You hear words at a comfortable volume-usually 25-40 dB above your threshold-and repeat them. Normal scores are 90-100%. If you score below 70%, you have poor speech discrimination. That’s common with cochlear damage or auditory nerve tumors. You might hear someone talking, but the words sound muffled or jumbled.
This is why two people with the same decibel loss can have very different experiences. One hears fine in quiet rooms. The other struggles even with family members. Speech testing explains why.
Tympanometry and Other Tests
Tympanometry checks your eardrum’s movement. A tiny probe seals your ear canal and changes the air pressure. It measures how flexible your eardrum is and whether fluid is behind it. A flat line (Type B tympanogram) means fluid or a perforation. A normal curve (Type A) means your middle ear is healthy.
This test takes 5 seconds. No beeps. No buttons. Just a weird pressure feeling. It’s especially useful for kids with ear infections or adults with recurring ear fullness.
For babies, infants, or people who can’t respond reliably, doctors use Auditory Brainstem Response (ABR). Electrodes on the scalp record how your brainstem reacts to clicks or tones. It’s objective-no need for you to press a button. It’s the gold standard for newborn screening.
Who Needs Audiometry Testing?
You don’t need to wait until you’re struggling to hear. Here’s when to get tested:
- You’re over 50-age-related hearing loss starts quietly.
- You work in loud environments-construction, factories, music, or aviation.
- You’ve had ear infections, head injuries, or take ototoxic meds (like some antibiotics or chemotherapy drugs).
- You notice ringing in your ears (tinnitus), muffled speech, or need to turn up the TV.
- You’re a parent-babies should be screened before one month old, with full testing by three months if they fail.
Many people ignore early signs. They think hearing loss is “just part of aging.” But untreated hearing loss is linked to social isolation, depression, and even faster cognitive decline. Catching it early means better outcomes with hearing aids or other support.
What Happens After the Test?
Your audiologist doesn’t just hand you a paper with lines and dots. They explain what the audiogram means. They’ll show you where your hearing dips-maybe at high frequencies, where women’s and children’s voices live. They’ll tell you if you need hearing aids, if your loss is temporary, or if you need to see an ENT doctor.
If you’re a candidate for hearing aids, they’ll match the device to your specific loss pattern. Not all hearing aids are the same. Some boost high frequencies better. Others reduce background noise. Your audiogram guides that choice.
Follow-up is important. Hearing can change. Most people get tested every 1-3 years, or sooner if they notice a difference. For those with occupational noise exposure, annual tests are required by law in many places.
Common Misconceptions
Some people think:
- “I don’t need a test because I can still hear loud sounds.” → But loud doesn’t mean clear. You might hear shouting but miss “p,” “t,” or “s” in conversation.
- “Retail hearing tests are good enough.” → Screening apps or kiosks can flag issues, but they can’t diagnose type or severity. Only a licensed audiologist can do a full diagnostic test.
- “Hearing aids fix everything.” → They help, but they don’t restore normal hearing. Speech training and listening strategies are often needed too.
Another myth: bone conduction testing hurts. It doesn’t. It feels like a vibration. Some people with glasses feel pressure behind the ear, but it’s brief and harmless.
What to Expect During Your Visit
Arrive with clean ears-no wax buildup. If you’re unsure, ask your doctor to check before the test. Bring a list of medications. Some antibiotics and diuretics affect hearing.
Wear comfortable clothes. You’ll sit in a soundproof booth. The audiologist will explain each step. You’ll hear tones, words, and feel pressure changes. No needles. No pain. Just quiet listening.
Afterward, you’ll get a printed audiogram and a clear explanation. If you’re confused, ask again. Good audiologists don’t just give you data-they help you understand it.
Where to Get Tested
You can get audiometry testing at:
- Hospitals and ENT clinics
- Dedicated audiology practices
- Some hearing aid centers (ask if they’re licensed audiologists, not just salespeople)
- Through workplace hearing conservation programs
Tele-audiology is growing, especially after 2020. Some clinics now offer remote testing using calibrated headphones and video guidance. But for full diagnostic testing, in-person is still best. Remote tests can’t do bone conduction or tympanometry reliably.
Why This Matters
Hearing loss affects 48 million Americans-and millions more worldwide. It’s not just about missing conversations. It’s about staying connected to family, keeping your job, and avoiding loneliness. Audiometry isn’t just a test. It’s the first step toward reclaiming your hearing-and your life.
Don’t wait until you’re shouting to be heard. If you’ve ever thought, “I think I’m losing my hearing,” get tested. It takes less than 30 minutes. The results could change everything.


Yash Hemrajani
November 27 2025So let me get this straight-you need a $500 machine to tell me I can't hear my cat sneeze? Meanwhile, my phone app says I have perfect hearing and recommends a 90s remix playlist. 🤦♂️