Many people confuse asthma and COPD because both make it hard to breathe. You might wheeze, feel tight in the chest, or cough nonstop. But these are two very different diseases - and treating them the same way can be dangerous. If you or someone you care about is struggling with breathing problems, knowing the difference isn’t just helpful - it’s critical.
What’s Really Happening in the Lungs?
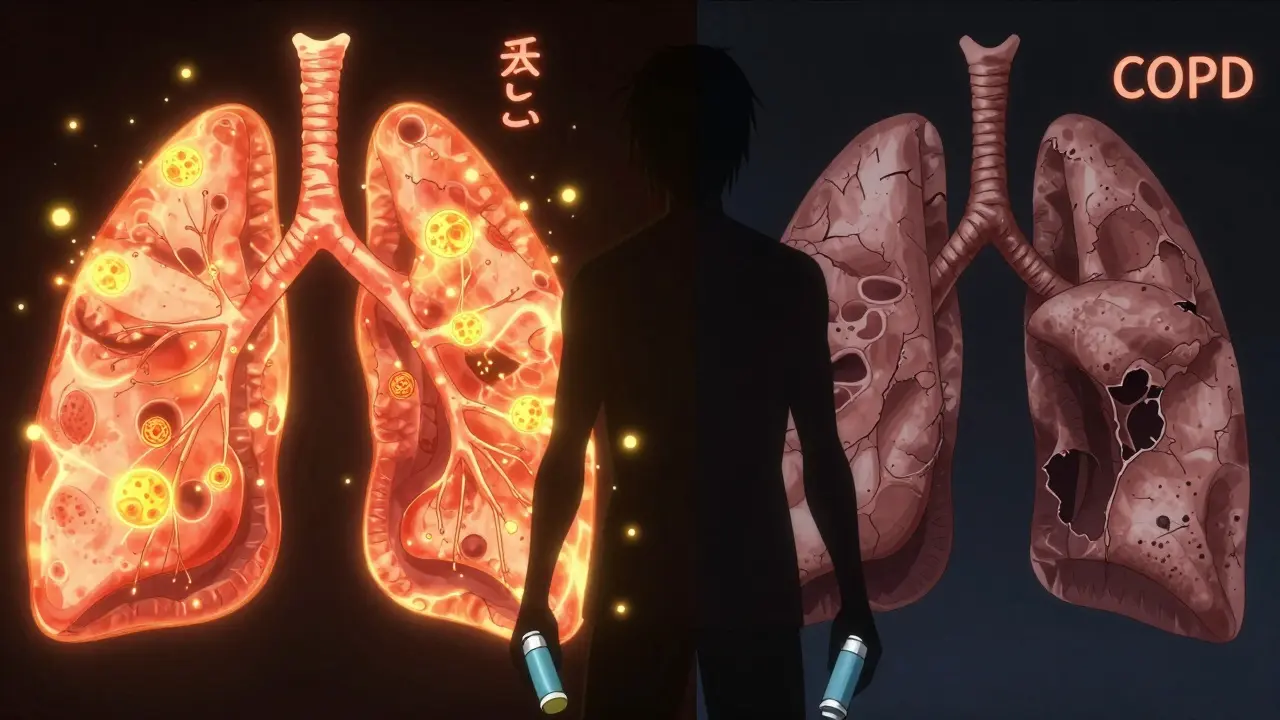
Asthma is an inflammatory condition where your airways react strongly to triggers like pollen, cold air, or exercise. When exposed, the muscles around the airways tighten, swelling and mucus build up, and breathing becomes a struggle. But here’s the key: between attacks, many people with asthma feel completely normal. Their lungs return to baseline. That’s why asthma is often called a reversible disease.
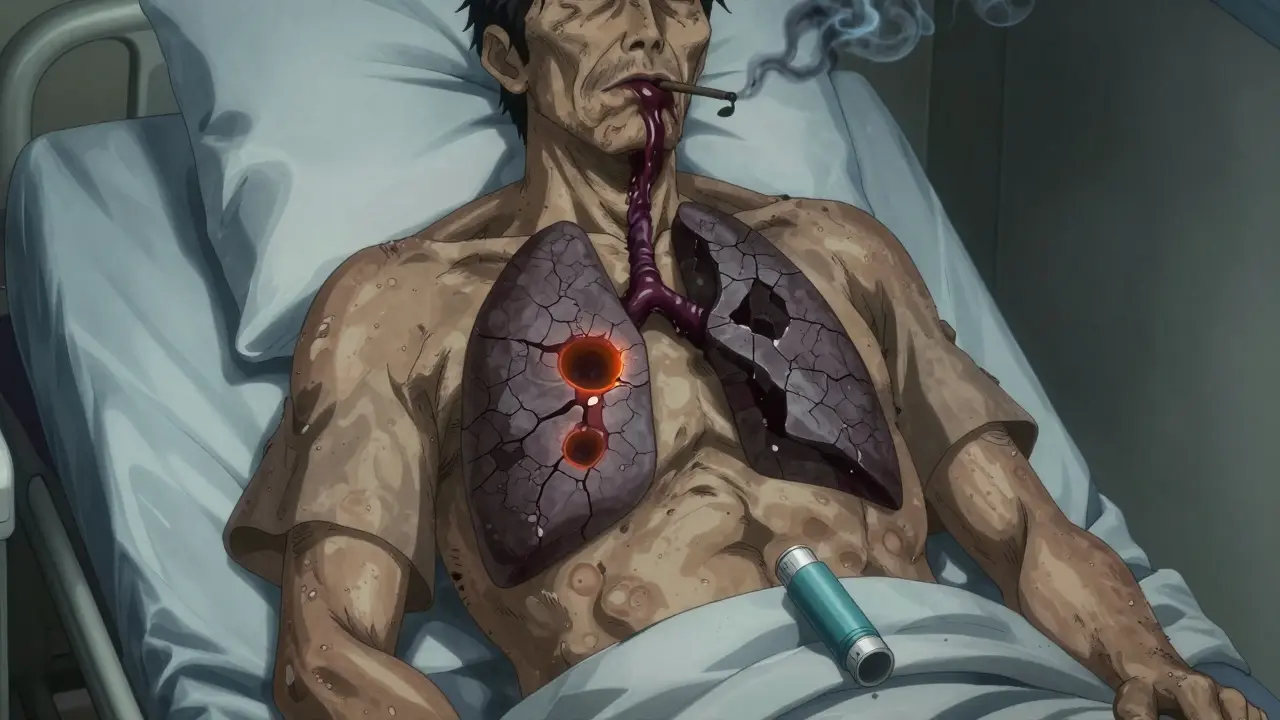
COPD - which includes emphysema and chronic bronchitis - is different. It’s not about sudden reactions. It’s about permanent damage. Years of smoking or long-term exposure to fumes and pollution destroy the tiny air sacs in the lungs (alveoli) and thicken the airway walls. The damage doesn’t heal. Airflow doesn’t bounce back. Even when you feel okay, your lungs are still working harder than they should.
How the Symptoms Feel Different
Let’s talk about what you actually notice day to day.
If you have asthma, your cough is usually dry. You might wake up at 3 a.m. with chest tightness. Wheezing happens mostly after exercise or when the weather changes. Symptoms come and go. Some people go weeks or months without trouble. A 2022 study found that 68% of asthma patients have long symptom-free periods.
COPD doesn’t take breaks. You’re likely to have a daily cough that brings up phlegm - thick, often yellow or green. Breathing gets harder over time, not just during flare-ups. By the time most people are diagnosed, they’ve been struggling for years. You might notice your lips or fingernails turning slightly blue (cyanosis) because your body isn’t getting enough oxygen. That’s rare in asthma.
Age matters too. Asthma often starts in childhood. Half of all cases are diagnosed before age 10. COPD? Almost never. Nine out of ten cases are in people over 45. If you’re 30 and having trouble breathing, it’s far more likely to be asthma than COPD.
Testing: What the Doctors Look For
Your doctor won’t just guess. They’ll use tests to tell them apart.
The gold standard is spirometry - a simple breathing test. You blow hard into a tube. The machine measures how much air you can force out in one second (FEV1). Then you inhale a bronchodilator - a quick-acting inhaler that opens airways. You repeat the test.
If your FEV1 improves by 12% or more after the inhaler, it’s likely asthma. About 95% of asthma patients show this kind of reversibility. If it barely changes? That’s a red flag for COPD. Only 15% of COPD patients show any real improvement.
Another tool is fractional exhaled nitric oxide (FeNO). This test measures how much nitric oxide is in your breath. High levels (above 50 ppb) mean your airways are inflamed by eosinophils - a type of white blood cell common in asthma. COPD patients usually have levels below 25 ppb. Blood tests for eosinophils help too. Counts above 300 cells/μL point to asthma or overlap. Below 100? More likely pure COPD.
CT scans show even more. In 75% of COPD patients, you’ll see holes in the lung tissue from emphysema. In asthma? Only 5% show that.
How Treatment Is Completely Different
Because the causes are different, the treatments can’t be the same.
Asthma treatment starts with quick-relief inhalers - usually albuterol - for sudden attacks. If you’re having symptoms more than twice a week, you’ll likely need a daily inhaled corticosteroid to calm the inflammation. For severe cases, newer biologic drugs like omalizumab or mepolizumab target specific immune pathways. These aren’t just pills - they’re injections that reduce flare-ups by up to 50% in people with allergic asthma.
COPD treatment? It’s all about long-acting bronchodilators. You’ll use either a LABA (long-acting beta-agonist) or a LAMA (long-acting muscarinic antagonist) every day - sometimes both. Inhaled steroids? Only if you’re having frequent flare-ups. They don’t fix the damage. They just help reduce inflammation that makes things worse.
Here’s the kicker: 89% of asthma patients can get their symptoms under control with proper meds. Only 52% of COPD patients feel they have good control. Why? Because you can’t reverse the scarring. You can only slow it down.
Pulmonary Rehab: One Works, the Other Doesn’t
Many people think pulmonary rehab is the same for both. It’s not.
COPD patients who do rehab - breathing exercises, walking programs, strength training - improve their walking distance by an average of 54 meters in six minutes. That’s huge. It means they can get through the grocery store without stopping.
Asthma patients? They gain only about 12 meters. Why? Because their lungs are already mostly fine between attacks. Rehab helps them stay fit, but it doesn’t fix a broken system like it does in COPD.
The Gray Area: Asthma-COPD Overlap Syndrome (ACOS)
Here’s where it gets messy. About 15-25% of people with obstructive lung disease have features of both. This is called ACOS.
These patients might have lifelong asthma but also a 30-year smoking history. They wheeze like asthma, but their airflow doesn’t fully reverse. They have high eosinophils (like asthma) but fixed airway damage (like COPD). Their symptoms are worse than either condition alone.
ACOS patients go to the ER 1.8 times a year on average - more than either asthma or COPD alone. Doctors often treat them with triple therapy: two long-acting bronchodilators plus an inhaled steroid. But evidence is still limited. It’s a work in progress.
Prognosis: What You Can Expect
Life expectancy tells a clear story.
If you have moderate asthma, your 10-year survival rate is 92%. For moderate COPD? It drops to 78%. That gap comes from the fact that COPD doesn’t just affect your lungs. It’s tied to heart disease, osteoporosis, and muscle loss. Smoking is the main driver - 90% of COPD cases are linked to it. In asthma? Only 20% are tied to smoking. Genetics play a bigger role.
But quitting smoking makes a massive difference. If you have COPD and quit, you cut your disease progression in half. That’s not a myth - it’s from the Lung Health Study. For asthma, quitting doesn’t change much unless you also have COPD.
What to Do If You’re Not Sure
Don’t wait. If you’ve been told you have one condition but your symptoms don’t match - or if your treatment isn’t working - ask for a second look. Misdiagnosis is still common. About 30% of people over 40 with breathing problems get the wrong diagnosis.
Ask your doctor about FeNO testing, blood eosinophils, and a repeat spirometry after bronchodilator. If you’re over 45, have a long smoking history, and your cough is always productive - don’t assume it’s just asthma. Get a CT scan. If you’re younger, have allergies, and your symptoms come and go - don’t ignore them because you think you’re "just out of shape."
The sooner you know what you’re dealing with, the better your quality of life will be.
Can asthma turn into COPD?
Asthma doesn’t automatically turn into COPD. But if you have asthma and smoke - especially for many years - you’re at higher risk of developing COPD on top of it. About 15-20% of people with long-term asthma (over 20 years) develop fixed airflow limitation, which looks like COPD. This is why quitting smoking is critical, even if you’ve had asthma since childhood.
Is it possible to have both asthma and COPD?
Yes. This is called Asthma-COPD Overlap Syndrome (ACOS). It’s more common than people think - affecting 15-25% of people with obstructive lung disease. These patients often have a history of childhood asthma and a long smoking history. Their symptoms are more severe than either condition alone, and they need a combination of asthma and COPD treatments.
Do inhalers work the same for asthma and COPD?
No. For asthma, quick-relief inhalers (like albuterol) are the first line, followed by daily steroids to control inflammation. For COPD, long-acting bronchodilators (LABAs or LAMAs) are the foundation. Steroids are only added if you have frequent flare-ups. Using a steroid inhaler for COPD without a bronchodilator won’t help much - and can increase infection risk.
Why does my doctor test my blood eosinophils?
Eosinophils are white blood cells linked to allergic inflammation. In asthma, they’re often high. If your blood eosinophil count is above 300 cells/μL, it suggests your airway inflammation is more like asthma - even if you’re older or a smoker. Below 100? More likely pure COPD. This helps doctors choose the right treatment, especially when deciding whether to add steroids.
Can I outgrow asthma or COPD?
Some children outgrow asthma - especially if it’s mild and triggered by allergies. But adult-onset asthma rarely goes away. COPD? No. It’s progressive and irreversible. Even if you quit smoking, the lung damage stays. The goal isn’t to cure it - it’s to slow it down and manage symptoms so you can still live well.

