When your asthma won’t improve no matter how many inhalers you use, it’s time to ask: is this really about asthma-or is it about your allergies?
For many people with asthma, especially those who struggle with symptoms year-round, the root cause isn’t just inflamed airways. It’s allergens. Dust mites in your mattress. Pollen drifting through open windows. Pet dander clinging to your clothes. These aren’t just irritants-they’re triggers that keep your immune system on high alert, turning mild asthma into a daily battle.
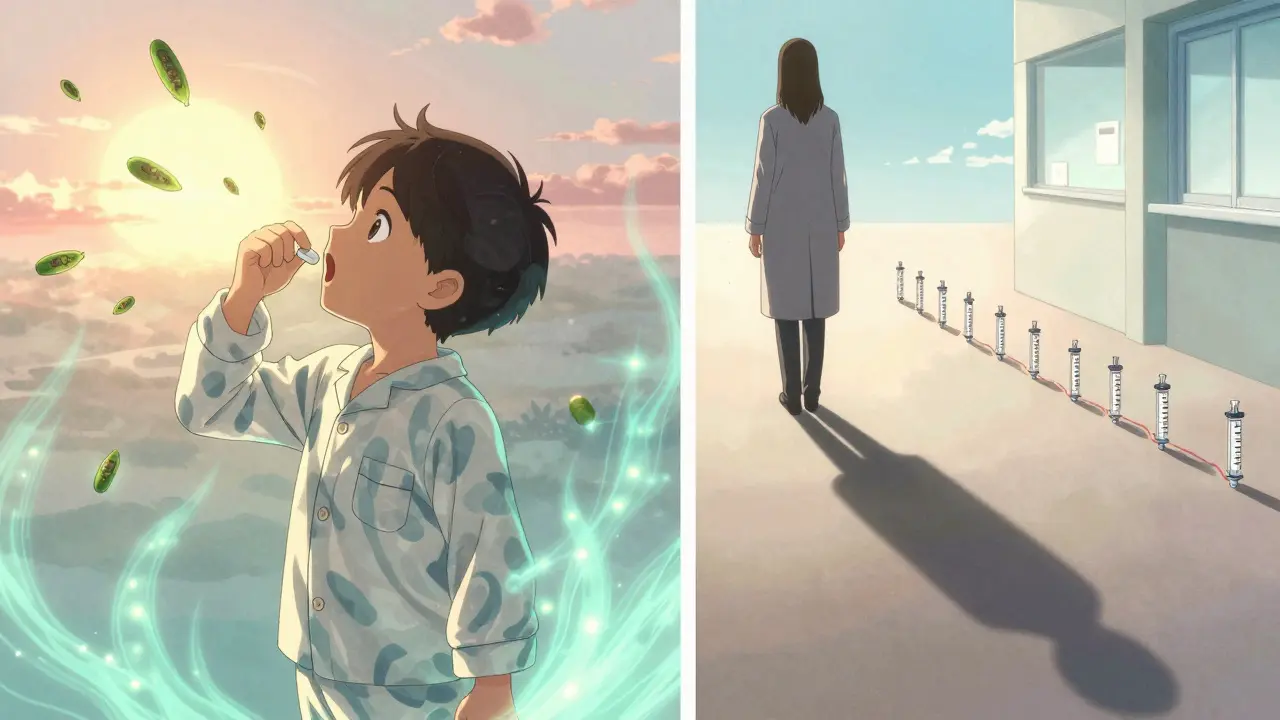
That’s where allergen immunotherapy comes in. Unlike inhalers that mask symptoms, immunotherapy rewires your immune system to stop overreacting. And for the past century, there have been two main ways to do it: allergy shots (subcutaneous immunotherapy, or SCIT) and allergy tablets (sublingual immunotherapy, or SLIT). Both work. But which one is right for you?
How Allergen Immunotherapy Actually Works
Think of your immune system like a security guard who’s been trained to panic at harmless things-like pollen or dust mites. Allergen immunotherapy slowly reprograms that guard. You’re given tiny, controlled doses of the exact allergen causing your asthma. Over time, your body learns: this isn’t a threat. No need to trigger wheezing, coughing, or tightness in the chest.
This isn’t just symptom relief. It’s disease modification. Studies show people who complete a 3- to 5-year course of immunotherapy often see fewer asthma attacks, less need for steroid inhalers, and even lower chances of developing new allergies. One major study found that kids with allergic rhinitis who got immunotherapy were 80% less likely to develop asthma later on.
The key? It only works if you’re allergic to something specific. If your asthma flares up every time you vacuum, dust mites are likely the culprit. If it gets worse in spring, grass or tree pollen might be the trigger. Skin tests or blood tests can confirm this. Without knowing the exact allergen, immunotherapy won’t help.
Allergy Shots: The Classic Approach
Allergy shots have been around since 1911. They’re the original form of immunotherapy. You go to a clinic, usually once a week at first, and get a small injection under the skin in your upper arm. The dose slowly increases over 3 to 6 months-this is the build-up phase. Then you switch to monthly shots for 3 to 5 years.
It’s a time commitment. Over the full course, you’ll likely need 50 or more visits. But for many, it’s worth it. Studies show SCIT reduces asthma symptoms significantly, especially for dust mite and pollen allergies. One landmark study with 36 patients showed clear improvement in both asthma and nasal symptoms after just one year of shots.
The biggest downside? Risk. About 1 in 10 people get a local reaction-redness, swelling at the injection site. Rarely, about 1 in 2,000 doses causes a systemic reaction: trouble breathing, dizziness, low blood pressure. That’s why shots are always given in a medical setting, and you have to wait 30 minutes after each one.
It’s not ideal for busy people. Missing a shot delays progress. Traveling? You need to plan ahead. But for those who can stick with it, the results are lasting. Many patients report breathing easier even years after stopping treatment.
SLIT Tablets: The Daily Alternative
SLIT tablets-like ACARIZAX for dust mites or GRAZAX for grass pollen-are a game-changer. Instead of needles, you place a small tablet under your tongue and let it dissolve for 1 to 2 minutes. Then you swallow. No needles. No clinic visits after the first dose.
The first dose is always supervised by a doctor. Why? Because, like shots, there’s a small risk of a systemic reaction-especially the first time. But after that, you can take it at home, in the morning before breakfast, every single day.
It sounds simple. But consistency is everything. Miss a day, and you lose momentum. The full course still takes 3 to 5 years. But because you don’t need to drive to a clinic, adherence is better. Studies show about 75-80% of people stick with SLIT, compared to 60-65% for shots.
And the results? Just as strong. A 2024 study found patients using the highest-dose HDM tablet reduced their inhaled corticosteroid use by 42%-nearly double the reduction seen in placebo groups. That’s not just symptom control. That’s medication independence.
Local side effects are common but mild: itchy mouth, throat irritation, or stomach upset. These usually fade after a few weeks. Serious reactions are rare-about 1 in 10,000 doses. And unlike shots, you don’t need to sit around waiting after each dose.

Shots vs. Tablets: The Real Differences
Here’s what actually matters when choosing between them:
| Feature | Subcutaneous Immunotherapy (Shots) | Sublingual Immunotherapy (Tablets) |
|---|---|---|
| Administration | Injection in clinic | Tablet under tongue at home |
| Frequency | Weekly (build-up), then monthly | Daily |
| Total visits over 3 years | ~50+ | 1 (initial supervision) |
| Best for allergens | Dust mites, pollen, mold, pet dander | Dust mites (ACARIZAX), grass pollen (GRAZAX) |
| Systemic reaction risk | Higher (~1 in 2,000 doses) | Lower (~1 in 10,000 doses) |
| Local side effects | Swelling/redness at injection site | Itchy mouth, throat irritation |
| Adherence rate | 60-65% | 75-80% |
| Reduction in steroid use | 30-40% | Up to 42% |
| Cost (out-of-pocket, Australia) | Higher due to clinic visits | Lower long-term, but tablet cost per month higher |
Both reduce asthma attacks. Both cut medication use. But SLIT wins on convenience. Shots win on flexibility-you can treat multiple allergens in one series. SLIT is limited to one allergen per tablet. If you’re allergic to both dust mites and grass pollen, you might need two different tablets, or stick with shots.
Who Should Avoid Immunotherapy?
Not everyone is a candidate. If you have severe, uncontrolled asthma (GINA Step 4 or 5), immunotherapy is risky. Your airways are already too inflamed. Starting this treatment could trigger a dangerous reaction.
Also, if your asthma isn’t allergy-driven-say, it’s triggered by cold air, exercise, or smoke-immunotherapy won’t help. You need proof of IgE-mediated allergy. That means a positive skin test or specific IgE blood test for at least one allergen.
People with autoimmune diseases, certain heart conditions, or those taking beta-blockers should talk to their doctor first. And while SLIT is approved for adults and children over 5, shots are generally preferred for younger kids because they’re easier to monitor.
What Real Patients Say
One Melbourne mum, Sarah, switched from daily steroid inhalers to SLIT tablets after her 7-year-old son’s asthma flared every time they cleaned the house. "We thought it was dust. Turns out, it was dust mites. The first month was weird-mouth itching every day. But after three months, he didn’t need his rescue inhaler at night anymore. Now, two years in, he’s off all preventers. No more missed school days."
On the other hand, Mark, 42, chose shots because he’s allergic to pollen, dust mites, and cat dander. "I hated the idea of needles. But I needed all three allergens covered. The shots took time, but I didn’t have to remember a daily pill. I just showed up every month. Now, I don’t even need antihistamines in spring."
Both stories are real. Neither is better-just better for them.
What’s Next for Allergen Immunotherapy?
Research is moving fast. Scientists are working on faster protocols-maybe cutting treatment from 5 years to 2. New adjuvants (additives that boost immune response) could make tablets more powerful. And there’s talk of combination therapies-like pairing SLIT with a low-dose biologic for stubborn cases.
But right now, the biggest barrier isn’t science. It’s access. In Australia, SLIT tablets are approved and available, but not always covered by PBS. Shots are more widely available through allergists, but require ongoing appointments. Many patients give up because of cost or logistics.
The bottom line? If you’ve tried everything and your asthma still won’t settle, immunotherapy isn’t a last resort-it’s the only treatment that can change the course of your disease. You’re not just treating symptoms. You’re retraining your immune system.
Start with testing. Find your trigger. Then talk to an allergist. Whether it’s a shot or a tablet, the goal is the same: breathe easier-for good.
Are allergy shots or SLIT tablets better for asthma?
Both are effective for allergic asthma, but they work differently. Allergy shots (SCIT) can treat multiple allergens at once and have slightly broader allergen coverage. SLIT tablets are easier to take at home and have a better safety profile, with fewer serious reactions. For dust mite allergies, SLIT tablets have shown up to a 42% reduction in steroid use-sometimes better than shots. The best choice depends on your allergens, lifestyle, and ability to stick with daily or weekly treatment.
Can SLIT tablets replace my inhaler?
SLIT tablets don’t replace rescue inhalers during an asthma attack. But they can reduce how often you need your daily preventer inhaler. Many patients cut their steroid inhaler use by 30-40% after 1-2 years of SLIT. The goal is long-term control, not instant relief. You’ll still need your inhaler for emergencies, but you may use it far less often.
How long does it take for immunotherapy to work?
You might notice small improvements after 6-12 months, but real, lasting results take 2-3 years. The full course is 3-5 years. Stopping early means you won’t get the long-term benefit. Many patients say their biggest win came after they stopped treatment-symptoms stayed gone for years.
Is SLIT safe for children?
Yes, SLIT tablets like ACARIZAX are approved for children as young as 5. Many parents prefer them over shots because they’re easier to administer and have fewer risks. Studies show SLIT reduces asthma attacks and school absences in kids with dust mite allergies. Always start under medical supervision, even for children.
Can I do immunotherapy if I have other health conditions?
It depends. If you have uncontrolled asthma, severe heart disease, or are on beta-blockers, immunotherapy may not be safe. Autoimmune diseases like lupus or rheumatoid arthritis also require caution. Always tell your allergist your full medical history. They’ll weigh the risks versus the benefits based on your individual case.
Will insurance cover allergy shots or SLIT tablets in Australia?
Allergy shots are usually covered under Medicare if you have a GP referral and see a specialist. SLIT tablets like ACARIZAX are listed on the PBS, but only for specific allergens and with strict criteria. You’ll still pay a co-payment, and not all brands are subsidized. Check with your allergist or pharmacist about current PBS eligibility before starting.
Next Steps: What to Do Now
If you’ve been struggling with asthma that won’t improve, start here:
- Get tested. Ask your GP for a skin prick test or specific IgE blood test to identify your triggers.
- See an allergist. Not all respiratory doctors specialize in immunotherapy. Find one who does.
- Ask about both options. Don’t assume one is better. Bring up SLIT tablets-even if your doctor hasn’t mentioned them.
- Consider your life. Can you commit to daily tablets? Or do you prefer fewer, scheduled clinic visits?
- Start before winter. Allergen exposure often spikes in colder months. Getting treated now means you’ll be better protected by flu season.
This isn’t a quick fix. But if you’ve been living with asthma for years, it might be the only thing that truly changes your future.


Enrique González
January 4 2026Been on SLIT for 2 years now. Dust mites were killing me. No more midnight coughing fits. No more dreading vacuum day. It’s not magic, but it’s the closest thing I’ve found to getting my life back. Worth every penny and every itchy mouth moment. 🌿